Foreword
The population of the UK is rapidly ageing and there are more people aged 65 and over than ever before. For most people, this means that they are spending more of their lifespan in good health, but recent data shows for the first time that disability-free life expectancy in the UK is falling and there are now more people with increasingly complex conditions towards the end of their lives who will need more specialist care.
Older people are the population group who use NHS and social care services the most. If we are to adequately care for this population, now and in the future, we need to care for the people who do the caring. There are not enough healthcare professionals specialising in older people’s healthcare and those who specialise in other areas may not always have the skills or training they need to care for their older patients. Although not evidenced in this report, we know from our members that the current workforce is exhausted and burnt out and a worrying proportion of them are moving towards retirement.
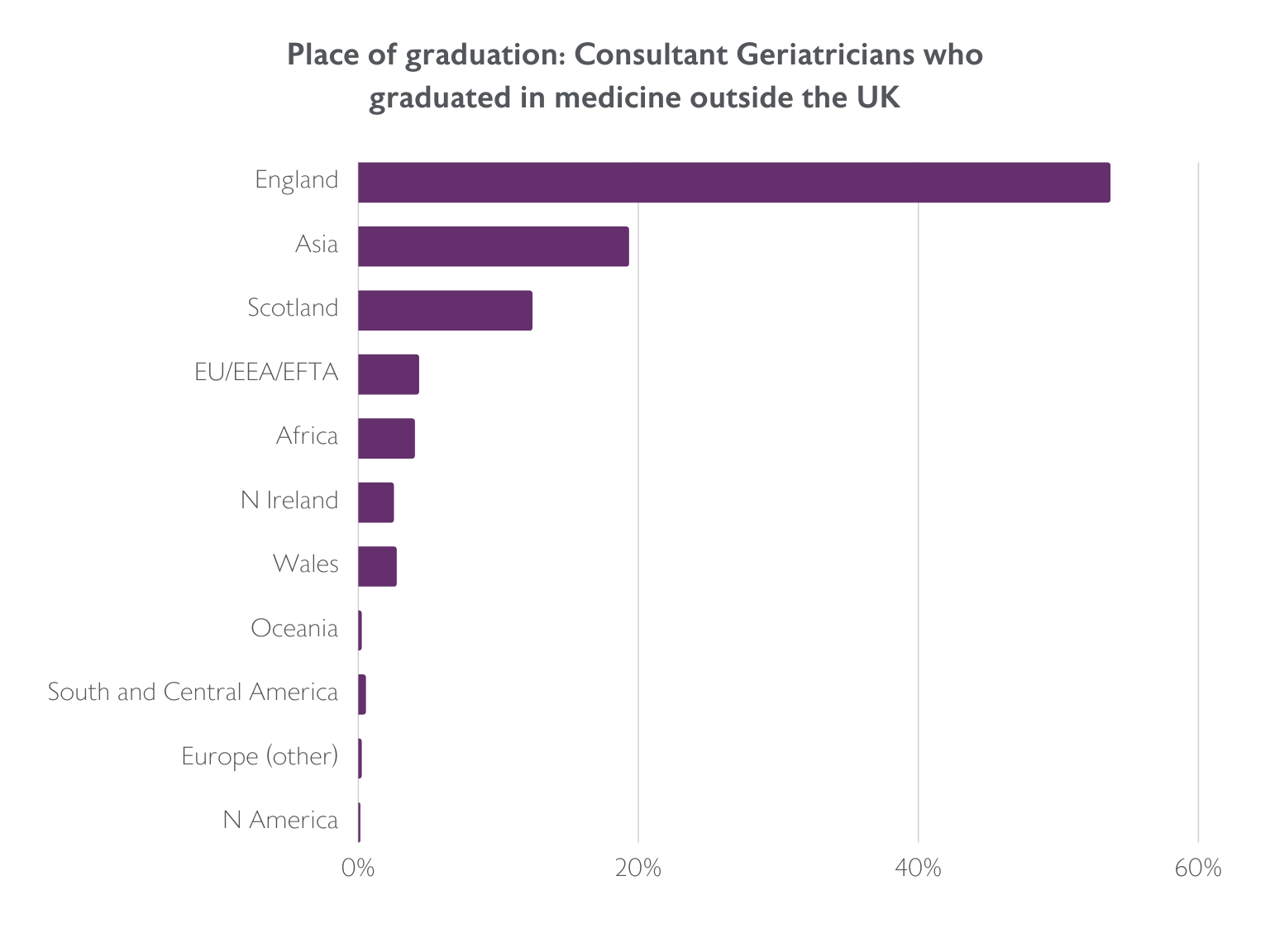
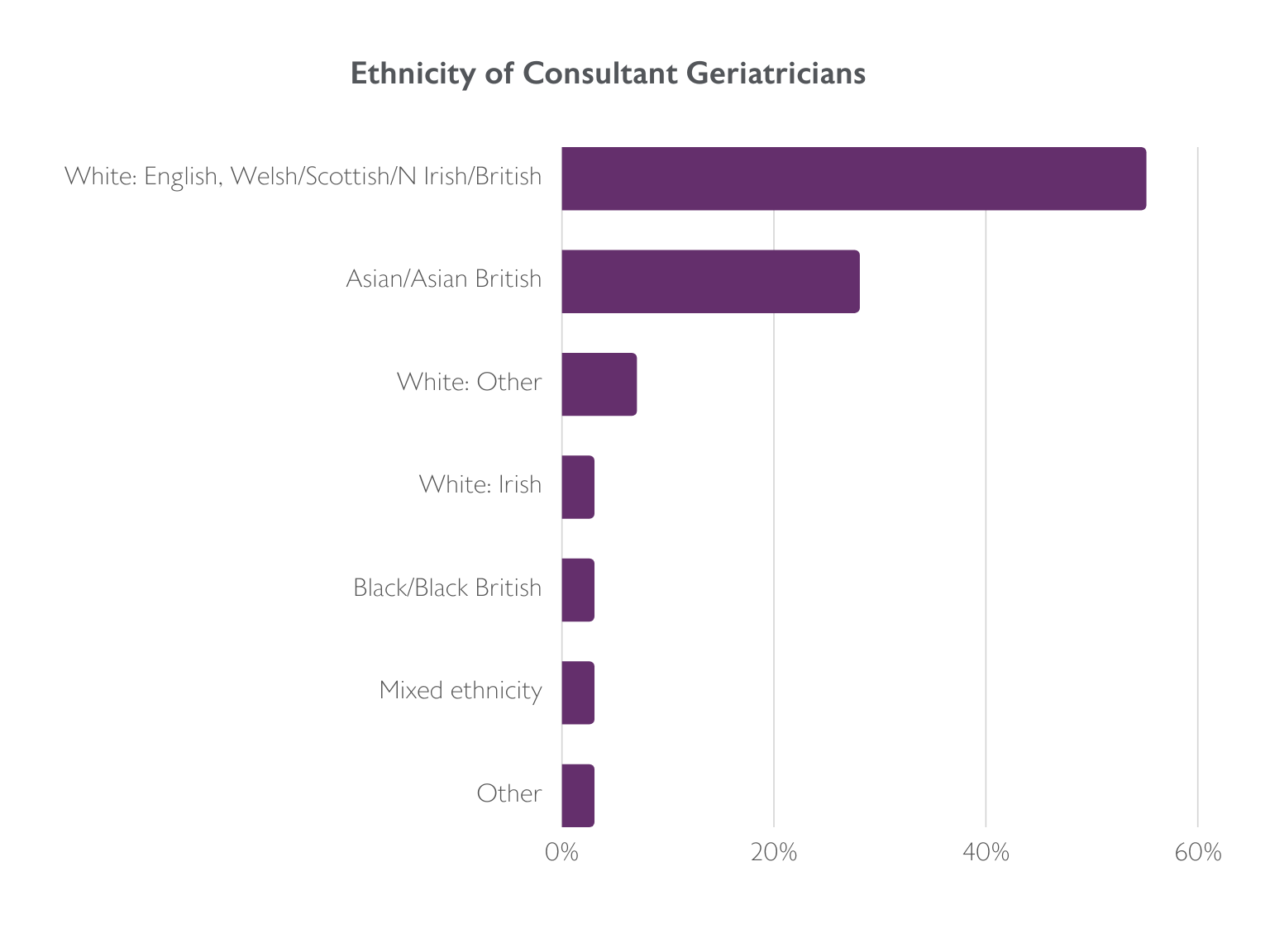
This report looks at data collected by the Royal College of Physicians on the consultant and Higher Specialty Trainee workforce. It paints a stark picture of the challenges facing older people’s healthcare. There are many unfilled consultant posts. Those in post deliver specialist care for older people living with frailty in hospital and in the community. They contribute significantly more to acute medicine on call and non-specialist inpatient care compared to some other medical specialties. Despite the growth in medical student places, there is still insufficient medical workforce being trained and retained to meet the needs of the population as it ages. We have much to do to influence training and career choices. Flexible training and working are established in this specialty and should be supported to maximise recruitment and retention.
This is however, only one part of the story. Older people’s healthcare is delivered by a multidisciplinary team across primary, secondary and community settings, and increasingly specialist expertise is needed to contribute to care closer to home. In order for the older people’s healthcare workforce to be adequately resourced, we need to consider the whole workforce and ensure that older people are placed at the centre of workforce planning.
Older people deserve no less.
Dr Jennifer Burns
BGS President
Dr Amit Arora
BGS Vice President for Workforce