Helen Wilson is an Orthogeriatrician at the Royal Surrey County Hospital in Guildford and has been working on Orthopaedic wards for more than ten years. She will be speaking at the BGS Autumn Meeting in the Living well with chronic disease session. She tweets occasionally @HelenWi72016310
How often is osteoarthritis named as a chronic disease on a GP summary or in a problem list forming part of a comprehensive geriatric assessment? Not infrequently perhaps but it certainly doesn’t feature as often as it should.
Osteoarthritis is very common in older people; diagnosed in half of over 65 year olds making it one of the most prevalent chronic diseases alongside hypertension (1). The consequence of untreated hypertension is well recognised by the public, causing morbidity and mortality by way of cardiovascular disease and stroke. But perhaps the increased mortality associated with osteoarthritis (SMR 1.5) is less known (2). General practitioners are incentivised through the quality outcomes framework to regularly review patients with many different chronic conditions but Osteoarthritis is not one of them.
NICE guidelines for Osteoarthritis care and management (CG177) have been in existence since 2008 and were updated in 2014 recommending a holistic approach, assessing the effect on a person’s function, quality of life and mood. Patient education and self-management are key in the early stages focusing on simple analgesia, heat and cold, exercise and weight loss (where appropriate). Physiotherapy assessment is often helpful, providing written guidance on strengthening exercises. NICE Guidelines also recommend annual review and referral for consideration of joint surgery if a patient has on-going symptoms that impact on their quality of life before there is functional limitation and severe pain.
Joint arthroplasty is accepted as a highly cost effective intervention in terms of cost per Quality adjusted life year (3). More than 215, 000 hip and knee replacements were performed in the UK in 2018. The mean age of patients was 68 years with 84% having an ASA grade of 1 or 2 (either healthy or with only mild systemic disease). For these patients surgery is usually uncomplicated with an average length of hospital stay of about 3 days.
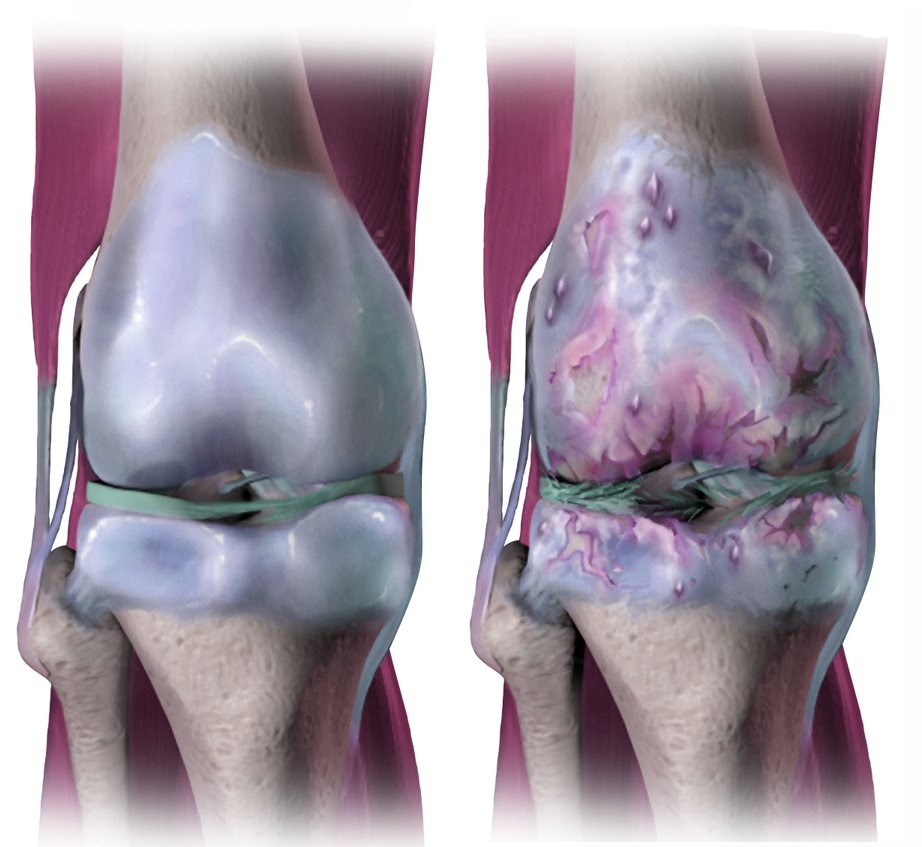
Osteoarthritis often starts in one joint but if managed inadequately can affect the whole body. There are many causes including trauma, repetitive use, genetic predisposition and inflammatory conditions. Wear and repair of articular cartilage leads to biochemical changes and degeneration. This then affects the subchondral bone with remodelling and cystic degeneration. There is an inflammatory process in the synovium and joint capsule leading to pain. Reduced elasticity in the ligaments can cause instability. Pain and loss of confidence result in reduced mobility with consequent muscle wasting. Avoidance of pain results in an antalgic gait altering the biomechanics of the spine and other joints. Musculoskeletal frailty ensues with a combination of osteoarthritis, osteoporosis and sarcopenia.
So is it too late for our patients with markers of frailty and functional limitations both as a result of their chronic arthritis and other co-morbidities? Exercise is still effective in individuals with frailty improving muscle strength, reducing sway, improving timed up and go and timed 4 metre walk (4). Pain is often difficult to manage, with simple analgesics ineffective and opiates offering minor benefit but associated with significant side effects. Joint arthroplasty in this group however, is a different prospect. The aims are not so much to prevent musculoskeletal frailty but to treat severe pain and enable some level of mobility. Patients should be reviewed in a Pre-operative assessment clinic with expertise in frailty to optimise their health status where possible. Whilst they often have greater peri-operative risk, this may be something that they feel is worth taking. A multidisciplinary approach is required with patients needing a longer period of rehabilitation (ideally at home) and considerable motivation to improve their mobility, often having become globally deconditioned. Setting realistic expectations is essential.
But looking to the future, as with osteoporosis and sarcopenia, the key to managing osteoarthritis is early identification, proactive management and follow-up to prevent musculoskeletal frailty.
1. A. Kingston, L. Robinson, H. Booth et al. Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age and Ageing, Volume 47, Issue 3, May 2018, Pages 374–380.
2. E. Nuesche, P. Dieppe, S. Reichenbach et al. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ 2011;342:d1165
3. P. Jenkins, N. Clement, D. Hamilton et al. Total hip and knee replacement: a cost utility analysis.
Orthopaedic Proceedings 2013, 95-B:SUPP 5, 8-8
4. N. Fairhall, C. Sherrington, S. Lord, et al. Effect of a multifactorial, interdisciplinary intervention on risk factors for falls and fall rate in frail older people: a randomised controlled trial. Age and Ageing, Volume 43, Issue 5, September 2014, Pages 616–62