The Geriatric Medicine Research Collaborative are very excited to declare that the first results of the “CovidCollab” study have now been published in Age & Ageing. This study was conducted by front-line trainees and clinicians working in the UK and internationally during the first wave of the global COVID-19 pandemic. Dr Carly Welch, who is nominally the Chair of the Geriatric Medicine Research Collaborative, tells us more about this study and what the results mean.
In March 2020, the World Health Organization declared the Coronavirus Disease 2019 (COVID-19) a global pandemic, and shortly after, the UK government put in place its first national lockdown to prevent the health service being overwhelmed due to the virus. Trainees across the country found themselves being redeployed as it became clear that more front-line clinical staff were needed. The Geriatric Medicine Research Collaborative (GeMRC) was established in 2017 as a trainee-led network for audit, research, and quality improvement. We had already successfully completed a number of other national projects, including our multi-centre delirium quality improvement project and delirium prevalence study. Trainees across the country contacted us to ask if we could “do something”. Despite this being an anxious time for all, we were astounded by the enthusiasm trainees expressed in wanting to harness this opportunity for research and improving patient care.
Realising that the clinical service requirements were likely to be great, we developed our study to ensure that it could be directly embedded into clinical care. We developed a simplified data collection tool, utilising data that could be collected by front-line clinicians from routinely-collected data. Early evidence from the pandemic suggested that age was associated with increased mortality with COVID-19, and we anticipated the importance of geriatric medicine research in enhancing our understanding of this. From the previous results of our delirium study, we immediately considered that research into COVID-19 should include the assessment of frailty and delirium. We were aware of challenging situations in Italy around the provision of critical care. Following the initial development of our protocol, the National Institute for Health and Clinical Excellence (NICE) produced guidelines that the Clinical Frailty Scale (CFS) should be performed routinely for patients admitted with COVID-19. We knew that research into factors that were predictive of mortality would be important, but also considered that other outcomes would be significant to older adults.
This project included routinely-collected data and only anonymised data was collected centrally. In line with Health Research Authority (HRA) guidelines, it was considered that data collection could be performed locally under the remit of service evaluation and/or audit against NICE guidelines, within the UK. However, we had also recently begun to develop international links, and we were encouraged by the success of the CovidSurg Collaborative in obtaining registration from international sites. We decided to open up registration to international sites. We were extremely fortunate that we were able to harness support from data administrators, academics, and statisticians with the Birmingham Centre for Observational and Prospective Studies (BiCOPS). This meant that whilst the protocol design, data collection, and manuscript preparation were all trainee-led, we were able to continue with our clinical commitments at the same time. Our data administrators supported site registrations, and the clarification of missing or outlying data, to ensure validity of our results. All data was anonymised, and uploaded via REDCap, which is a secure encrypted web-based programme for data collection. As is the case with all our publications, all collaborators who contributed towards this project have been listed as fully Pubmed-citable collaborative authors.
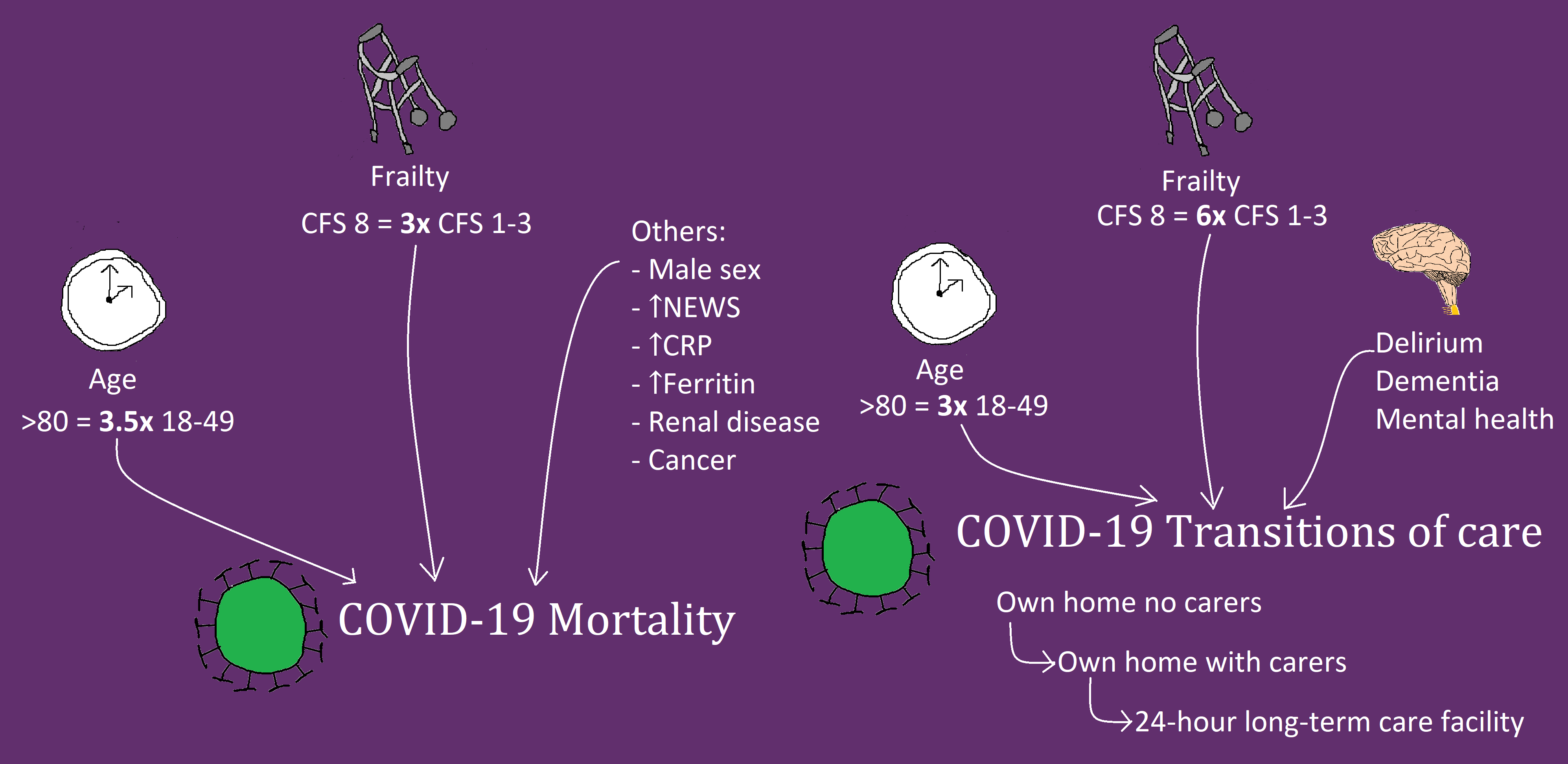
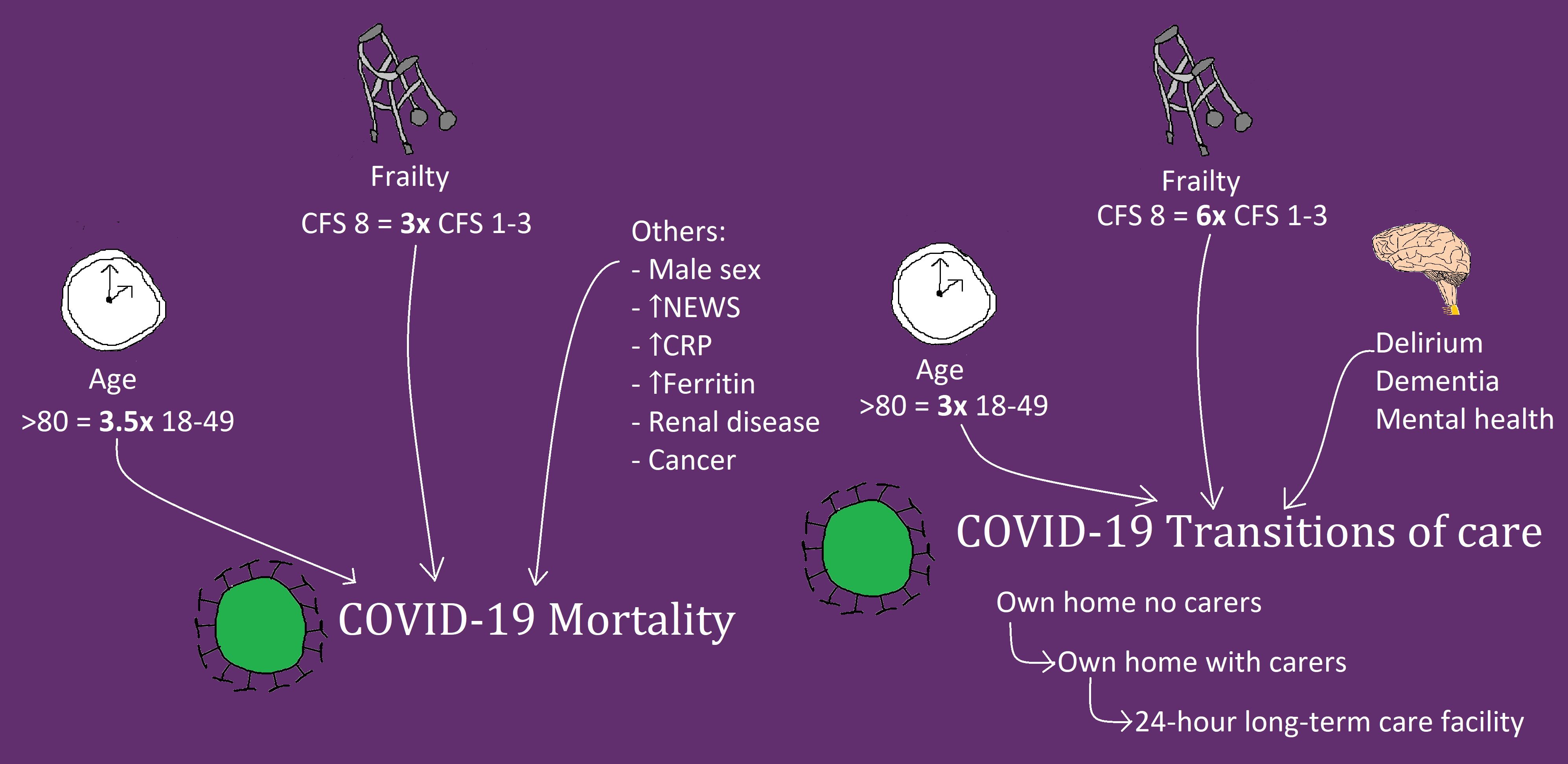
This study includes results from 5711 patients at 55 hospitals in 12 countries. As the pandemic has progressed, multiple other studies have considered the effects of frailty and delirium on mortality with COVID-19. These have shown conflicting results, but have been mainly single centre studies. Our study is the largest study performed to date that specifically assesses this relationship. Careful consideration and interpretation of our results demonstrate that both age and frailty are independently associated with increased risk of mortality in hospitalised patients with COVID-19. These results are important when we consider current advice on shielding and the Joint Committee on Vaccination and Immunisation recommendations for vaccine prioritisation. They also underline the importance of timely advance care planning decisions, considering the best interests and wishes of older people. Interestingly, although we have shown that delirium is extremely prevalent in patients with COVID-19, and indeed, may be the sole presenting feature in older adults, delirium itself was not independently associated with increased risk of mortality. We know that delirium presents as a marker of both frailty and illness severity, both of which were independently associated with increased mortality in our study.
Our study also presents novel results related to discharge destination in survivors of COVID-19. We have shown that there is an increased likelihood of transition to a higher level of care on discharge with increasing age, frailty, delirium, dementia, and mental health problems. Quality of life is individual and subjective, but for some, these transitions in care will have been hugely significant. We know that many hospitalised patients with COVID-19 of all ages experience extreme muscle atrophy and weakness, and many experience prolonged symptoms of fatigue and incomplete recovery. The phenomenon of acute sarcopenia is increasingly recognised as an acute organ insufficiency in hospitalised patients, and its prevalence with COVID-19 is considered to be high. Further research is needed to understand what factors affect recovery of physical function and quality of life with COVID-19, such as the Post-Hospitalisation COVID-19 (PHOSP-COVID) study. The inclusion of older adults with frailty in such research is paramount.
Above: Graphical representation of CovidCollab results presented in the main article. CFS = Clinical Frailty Scale; NEWS = National Early Warning Score; CRP = C-Reactive Protein
What is next for the Geriatric Medicine Research Collaborative?
We’re currently writing further papers using data from the CovidCollab project, so watch this space! Meanwhile, we also have other projects we’ll be planning in the future, and we welcome involvement from medical students, trainees, and allied health professionals, regardless of previous research experience. If you’re interested in getting involved, keep an eye on our website, get in touch with your regional representative, or email us at gemresearchuk@gmail.com.
A huge thank you goes to all our collaborators who contributed towards this project, without whom, none of this would have been possible!