Dr George Peck is a Consultant Geriatrician at St Mary’s Hospital, London, providing embedded medical care to the major trauma centre at Imperial College Healthcare NHS Trust. Dr Emily Feilding is a Consultant Geriatrician at Salford Royal NHS Trust, Manchester, providing medical care to the major trauma centre. Here they discuss the emerging role of geriatricians in the management of major trauma patients. Follow on twitter via @elderlytrauma and @fe7el
Major trauma was once perceived as a realm of vehicle accidents or violence affecting young or middle-aged people. The Trauma Audit and Research Network has now shown that the majority of patients attending hospitals with severe injuries are >60 years of age and have fallen from a standing height. Many of these patients have multi-morbidity and are complex to manage.
In 2012 trauma care across England changed dramatically with the development of regional trauma networks. Several satellite trauma units support a central major trauma centre with 24/7 access to multiple surgical specialties and interventional radiology. There are currently 27 major trauma centres across England and 4 in Scotland. Severely injured patients are taken directly to the major trauma centre where they can receive prompt high quality care. This has led to an impressive 20% reduction in mortality since the inception of the National Trauma Network in 2012. In the last decade it has become clear that major trauma centres are admitting an increasing number of complex older patients. Specialist geriatrician skills are needed to manage these patients effectively.
Orthogeriatric models of care have shown conclusively that geriatrician input in the management of vulnerable hip fracture patients can have significant positive effects on mortality, length of stay and quality of care. The role of geriatricians in the management of other surgical specialties is also now well established and is a rapidly growing sub-speciality.
Orthogeriatrics is closely linked to the National Hip Fracture Database which has incentivised Trusts across the NHS to provide geriatrician resource for older patients with fractured hips, but patients with other traumatic injuries have not had the same standard of care. The British Orthopaedics Association recently acknowledged this in their 2019 BOAST Standard suggesting that all patients with fragility fractures or major trauma should receive multidisciplinary input including ortho-geriatricians. This is not, however, yet associated with any tariff.
The National Trauma Network has gone one step further and introduced a Best Practice Tariff for major trauma centres in April 2019 worth in excess of £3000 per patient; all patients >65 years of age with major traumatic injuries must have a clinical frailty scale recorded by a geriatrician (ST3 or above) within 72 hours of admission.
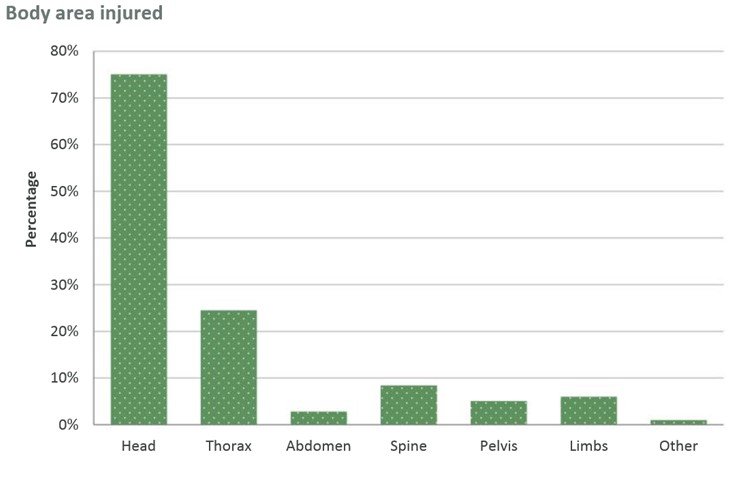
Whilst many older trauma patients have long bone injuries or fragility fractures, the most prevalent major traumatic injuries are in fact head injuries and blunt chest trauma (click here to see Figure 1). Alongside these, spinal injuries are prevalent and can be associated with significant spinal cord injury.