Guideline for the care of people living with frailty undergoing elective and emergency surgery that encompasses the whole perioperative pathway
The Centre for Perioperative Care, working in collaboration with the British Geriatrics Society, has published guidance for the care of people living with frailty undergoing elective and emergency surgery that encompasses the whole perioperative pathway.
Bringing together the multidisciplinary team to improve care for people living with frailty
Frailty is a condition characterised by loss of biological reserve, failure of physiological mechanisms and vulnerability to a range of adverse outcomes including increased risk of morbidity, mortality and loss of independence in the perioperative period. With the increasing recognition of the prevalence of frailty in the surgical population and the impact on postoperative outcomes, the Centre for Perioperative Care (CPOC) and the British Geriatrics Society (BGS) have worked together to develop a whole pathway guideline on perioperative care for people living with frailty undergoing elective and emergency surgery.
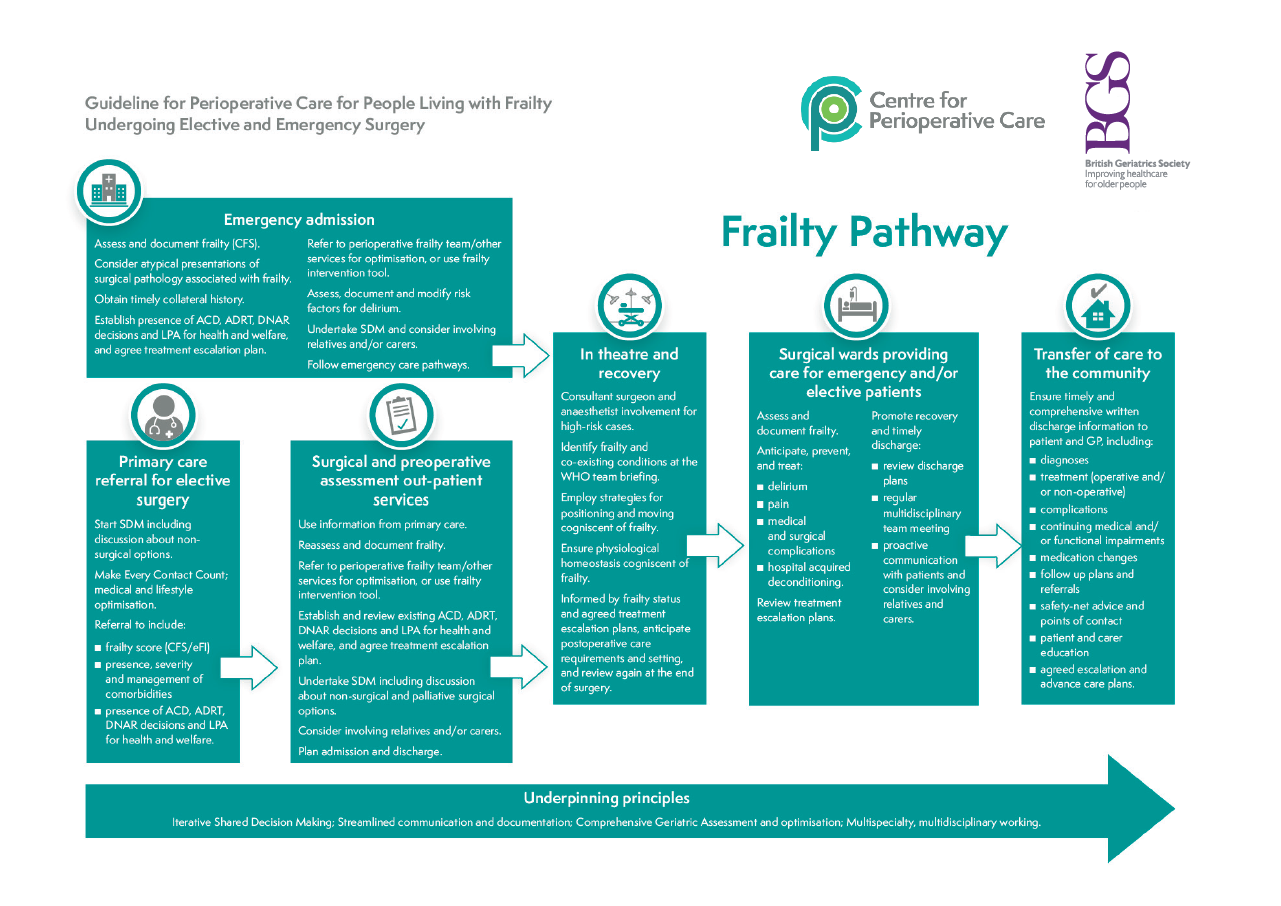
Delivering whole pathway, quality perioperative care requires multicomponent intervention, with integration across community, primary, secondary and social care. A multidisciplinary ‘one-team’ approach across these sectors is necessary to deliver each component of the pathway:
- Patient and carer involvement, education and empowerment
- Preoperative risk assessment and optimisation of physiological status, comorbidities and geriatric syndromes including frailty
- Lifestyle modification to improve both perioperative and long-term health outcomes
- Shared decision making (SDM)
- Optimal intraoperative surgical and anaesthetic management
- Quality postoperative care in the most appropriate setting to include rehabilitation
- Proactive discharge planning
- Links and referral to relevant community, primary care and follow up services
The scope of this guideline covers all aspects of perioperative care relevant to adults living with frailty undergoing elective and emergency surgery. It is written for healthcare professionals involved in delivering care throughout the pathway, as well as for patients and their carers, managers and commissioners. Implementation of the guideline will require collaboration across the four nations of the United Kingdom between all stakeholders, underpinned by an implementation strategy, workforce development with supporting education and training resources and evaluation through refinement of current national audit tools. We believe this is an important step in improving outcomes for our patients and healthcare services.
Structure of the Guideline
Perioperative care for people living with frailty is particularly complex and deficiencies in current perioperative pathways have been well described. Despite published interventions for frailty, an implementation gap between recommended care and routine perioperative practice exists. This may be a consequence of too few geriatricians, silo working and difficulties in embedding complex interventions for frailty in the clinical setting, compounded by unintended consequences of time-based targets (for example the 62 day cancer pathway) and a lack of commissioning incentives to embed a whole pathway perioperative team. To address this challenge, this new guideline has been coordinated by CPOC and the BGS, working with patient representatives and all stakeholders involved in the perioperative care of patients with frailty undergoing surgery.
- Standards
- Recommendations for people living with frailty and their carers
- Recommendations for commissioners and providers of surgical services for people living with frailty
- Recommendations for primary care teams
- Recommendations for staff working in surgical outpatients and preoperative assessment services
- Recommendations for staff working in surgical wards providing care for emergency and/or elective surgical patients
- Specific considerations in the emergency setting
- Recommendations for staff in theatre and recovery
- Recommendations for transfer of care to the community
- Recommendations for quality improvement and metrics
- Recommendations for Research
Download the guideline here.