What is care and support planning?
The Royal College of General Practitioners defines personalised care and support planning as:
“A powerful way of creating an environment which helps clinicians to support self-management by patients of their own long term condition.”
However a more holistic definition comes from the new NHS England Service Component Handbook on personalised care and support planning:
‘Personalised’ care and support planning is an essential gateway to better supporting people living with long term physical and mental health conditions, and carers, helping them to “develop the knowledge, skills and confidence to manage their own health, care and wellbeing.” It helps individuals and their health and care professionals have more productive conversations, focused on what matters most to that individual.
The term ‘personalised’ reflects that the “conversation relies on equal input from the individual and their carer, where appropriate, alongside health and care practitioner(s)” and looks at the individual’s health and care needs within the wider context of their lives. ‘Care and support’ signals that “people need more than medicine or clinical treatments and that social, psychological needs and support to do things for themselves are equally important,” alongside opportunities for community inclusion and support.
The essence of personalised care and support planning is:
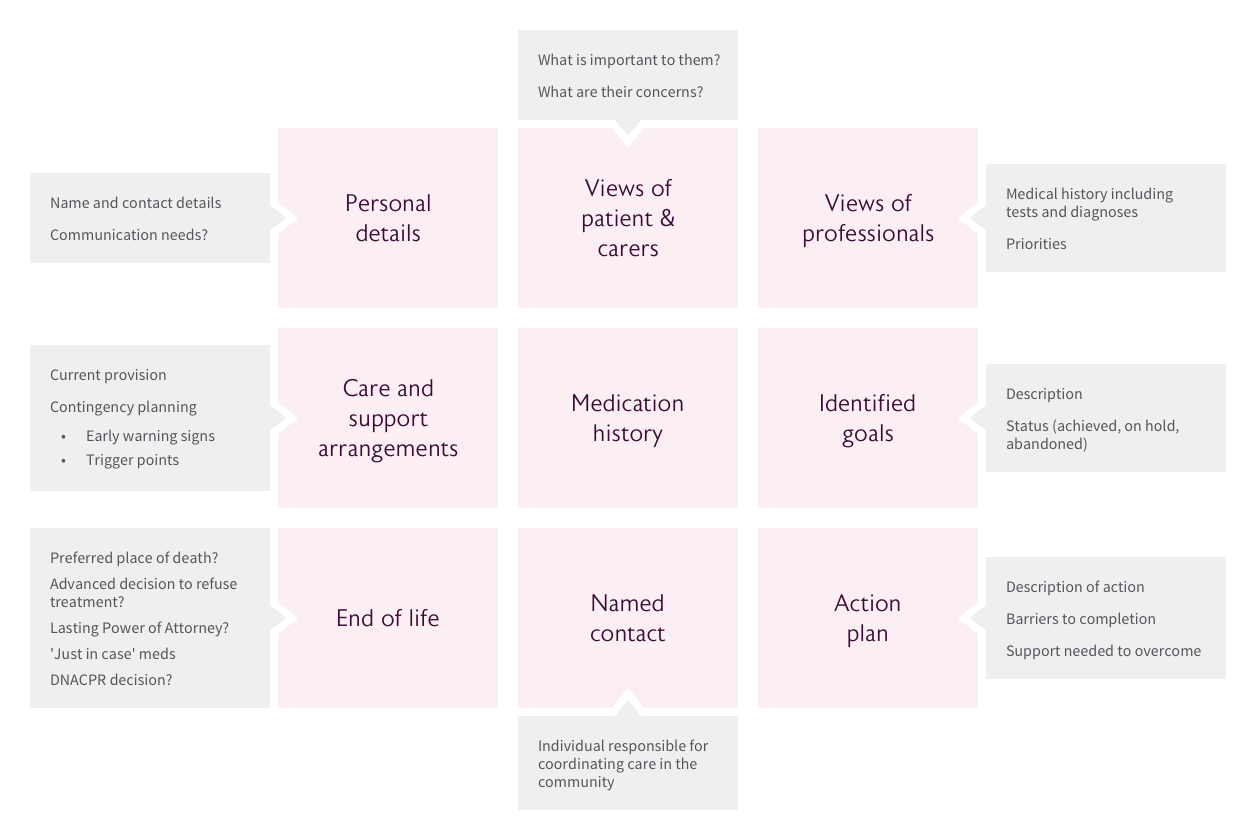
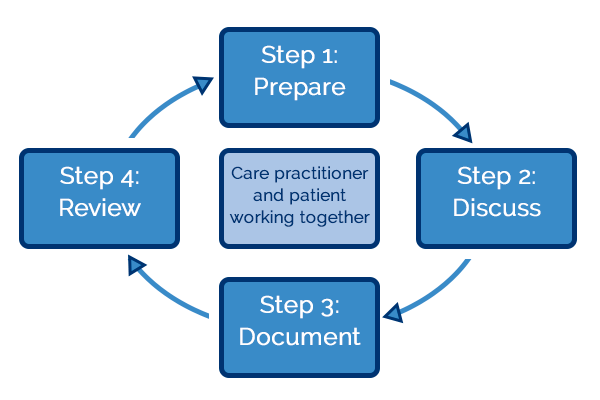
- A conversation between an individual (including their family/carer when appropriate) to discuss life priorities, consider options and agree goals.
- Working with the individual to identify the best clinical treatments and/ or social and psychological support for them, taking account of their life priorities and the agreed goals.
- Agreeing the actions individuals themselves will take to help them achieve their jointly agreed goals and the support they may need to do that.
- Recording the conversation in a way relevant to the individual.
- A planned and continuous process, not a one-off event.
There is a drive for care plans to be more widely implemented; the NHS Mandate included a commitment that by April 2015:
“Everyone with long-term conditions, including people with mental health problems, will be offered a personalised care plan that reflects their preferences and agreed decisions.”
The NICE Guidance for Older People with Multi Morbidity published in September 2016 recommends a care plan reviewed annually.
Why is it vital?
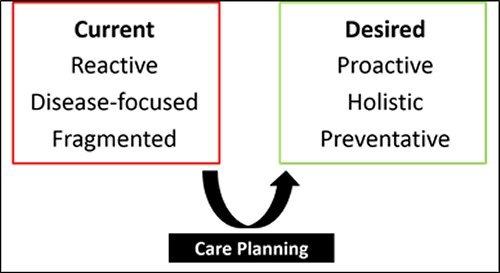
One of the most important challenges facing the 21st century NHS is the need to improve the treatment and management of long-term conditions, multi-morbidity and support and care for older people living with frailty. Part of the problem relates to how our models of care tend to be structured. Traditional models of care, which focus on the management of single long term conditions, do not fit the paradigm of care required for those living with multi-morbidity and frailty. It is recognised that change is needed. The term ‘house of care’ has been adopted as a central metaphor in NHS England’s plans for improving care for people with long-term conditions - care planning has been recognised as being at the very heart of this process of driving change (Figure 1, below).
In an age of austerity, it is worth noting that evidence suggests personalised care and support planning can produce the most appropriate use of limited healthcare resources.