To learn more about QI tools and methods, when one might be more appropriate than the other, and their pros and cons, the websites below provide advice and guidance:
- A Guide to Quality Improvement Tools – HQIP
Healthcare Quality Improvement Partnership’s guide introduces a variety of quality improvement tools used in healthcare and presents case examples and associated tools available to assist with implementation. Also includes an e-learning site with certificate on completion.
-
Royal College of Emergency Medicine (RCEM) provide a practical guide for clinicians undertaking quality improvement projects. It introduces the different tools and specifies: when to use it, how to use it, advantages and disadvantages along with examples.
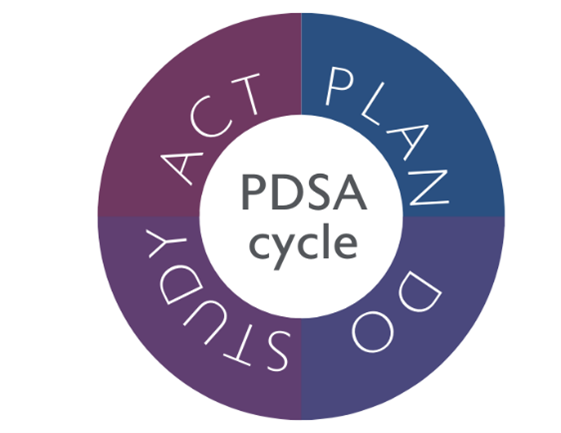
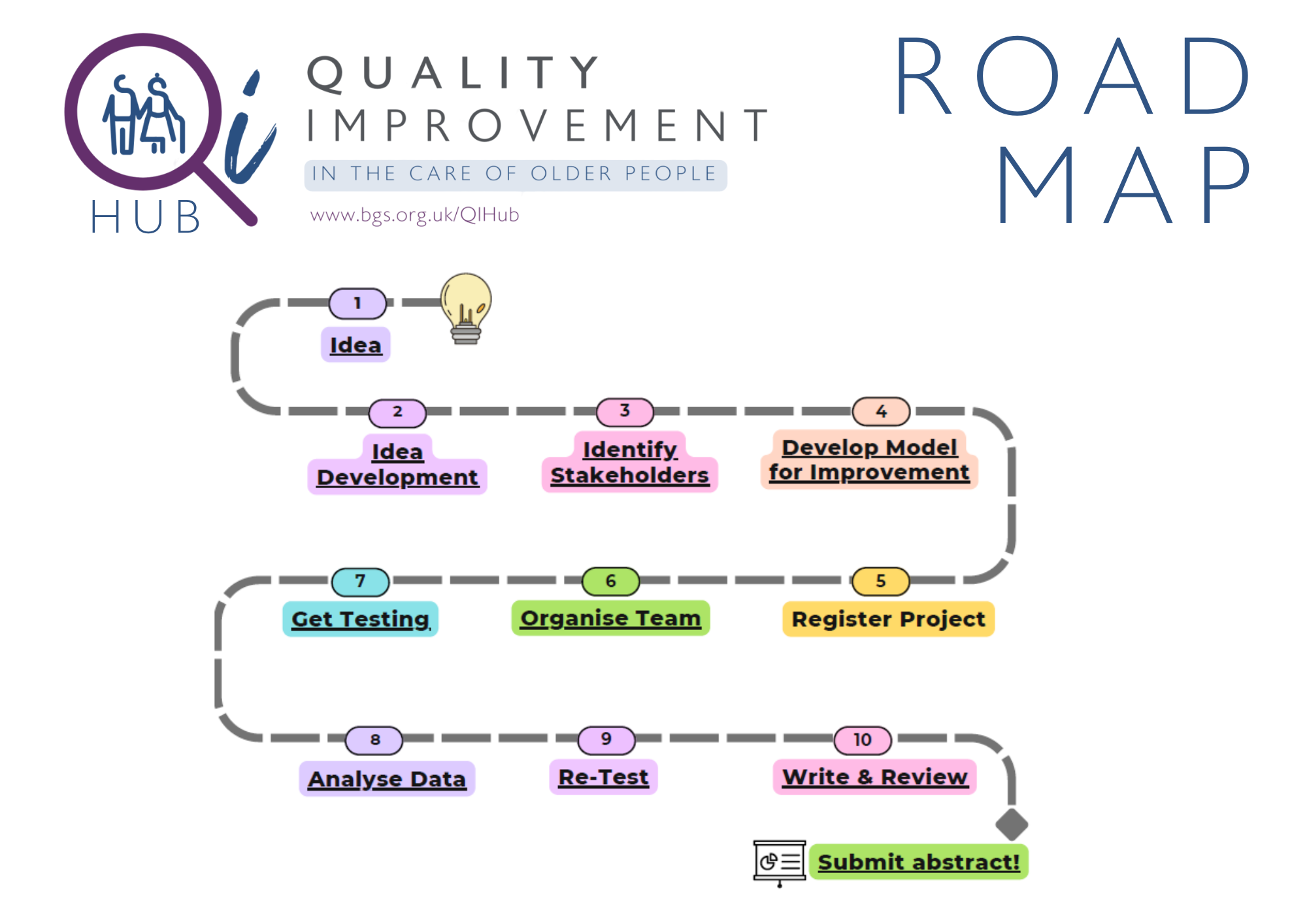
Model for improvement
This simple yet powerful model has been widely taught within the NHS. It underpins many of the QI change projects undertaken within the service and most of the poster presentations seen at BGS conferences.
This section will focus on the model for improvement as a method to drive improvement. It is more responsive than the traditional audit and allows a series of interventions to be tested, adapted and evaluated quickly, making it an effective way to influence culture and create change.
The following links provide a good starting point to find out more about this model:
-
The Improvement Guide: a practical approach to enhancing organizational performance - Langley G, et al. (2nd Edition) 2009
This book explains how the Model for Improvement works in improvement efforts at multinational companies as well as in different industries such as healthcare and public agencies.
-
Quality Improvement - Imperial College Healthcare NHS Trust
These videos explain in more depth how the Model for Improvement can be leveraged.
-
Testing changes: Quality Improvement Zone - TURAS (NHS Education for Scotland)
Animation giving an overview of Testing Changes.
-
Quality Improvement Resources - RCEM
This page collates some of the most useful quality improvement resources for emergency staff.
The Model for Improvement requires us to ask three important questions before anything is done:
1. What are we trying to achieve?
Developing an ‘aim’ statement
Aim setting is important and vital to the success of your project. Be prepared to work hard on this with your team. The aim must be measurable, clear and it must be understood by everyone involved in the project. The aim should be time-specific and it should also define the specific population of people, whether they be patients, staff or others, that will be benefitted by the improvement.
You may not get your aim statement right first time, but it is crucial not to start work on your project until you have a clear and measurable aim.
The below resources may be helpful in defining and refining an aim for your project:
- Setting Aims: Science of Improvement - IHI - (Institute for Healthcare Improvement)
Improvement requires setting aims. An organisation will not improve without a clear and firm intention to do so. Agreeing on the aim is crucial; so is allocating the people and resources necessary to accomplish the aim. This links provides helpful background, the 6 major quality improvement areas, and examples of effective aim statements.
- Tips for Setting Aims: Science of Improvement - IHI (Institute for Healthcare Improvement)
This link summarises five top tips for setting a project aim.
2. How will we know that a change is an improvement?
Developing aims and measures
Planning data collection
- Using data for improvement - BMJ (2019)
Really good article which talks about the role of qualitative and quantitative data for improvement, and how different types of data are needed based on what you’re measuring (outcome measures, process measures, balancing measures, etc).
- Making Data Count - NHS Improvement
This practical guide is suitable for those working at all levels in the NHS, from ward to board, and will show you how to make better use of your data
- The How-to Guide for Measurement for Improvement – NHS Improvement
This guide was designed to help to demonstrate if changes are really improvement, by testing changes and measuring the impact successfully. Part 1 explains what measurement for improvement is and how it differs from other sorts of measurement. Part 2 describes the process of collecting, analysing and reviewing data.
Run charts
- A Guide to Creating and Interpreting Run and Control Charts Turning Data into Information for Improvement - NHS Institute for Innovation and Improvement
A clear guide to analysis run charts. It provides guidance to ask the right questions and to better assess whether a change has led to an improvement.
- Run charts: Quality Improvement – NHS East London Foundation Trust
Step-by-step guide on how to make a run chart.
- Run Chart Part 2: Interpretation of Run Chart Data – Clinical Excellence Commission (Australia)
Australian (NSW Government) video on interpreting a run chart (17 mins in length).
Statistical process control/control charts
- How to use Statistical Process Control (SPC) charts: Quality Improvement - East London NHS Foundation Trust
Useful slides on how to use SPC charts
Different measures
- STEP 3: Process, outcome and balancing measures – East Lancashire Hospitals NHS Trust
One-slide definitions.
3. What changes can we make which will achieve our aim?
Selecting your tests of change
While not all changes lead to improvement, all improvement requires change. The ability to develop, test, and implement changes is essential for any individual, group, or organisation that wants to continuously improve.
Identifying changes to test is often the easiest part of an improvement project. Everyone will have ideas, but how do you choose the right ones and how can you structure your choices so that you are more confident the changes you test are the ones most likely to deliver the aim you wish to see?
- Science of Improvement: Selecting Changes - Institute for Healthcare Improvement (IHI)
Provides examples of change concepts.