As part of implementing Derbyshire Community Health Services NHS Foundation Trust Frailty Strategy, there was recognition that workforce capability is a crucial success factor. In addition, raising awareness across the Trust and Joined up Care Derbyshire (JucD) STP was an important step in meeting the demands of a changing population profile (which include ageing and multi-morbidity) as well as wider system priorities.
Against this backdrop, the decision was made to create a Specialist Lead Trainer post, which coincided with Skills for Health publication of the Frailty Core Capabilities Framework. The brief was to utilise the dementia, end of life and frailty core capabilities frameworks and develop a training programme which prepared staff for the increasing acuity, complexity and dependency among older people living with frailty in our local system and work towards achieving the ‘Quadruple Aim’.
Evidence suggests that both clinical and non-clinical healthcare professionals from across all disciplines need to be able to understand each other’s perspectives to work together safely and efficiently to deliver the highest quality of care, especially the care of older people living with frailty and/or multi-morbidity. This promotes a person-centred and integrated approach to delivering healthcare.
The Department of Health (2000) stated: “It is about looking at the workforce in a different way, as teams of people rather than as different professional tribes. For too long we have planned and trained staff in a uni-professional/uni-disciplinary way without a clear and comprehensive look at the future.”
Multi-disciplinary training is used in different professional disciplines and is a particularly useful approach when dealing with a subject area in which a team of professionals need to collaborate. End of life care, dementia and frailty are prime examples of where a co-ordinated, collaborative workforce training programme has the potential to drive forward teamwork. For this reason, it was foreseen that any training programme developed needed to be multi-professional and tiered to deliver training in a manner that is reflective of people's roles and responsibilities. The aim of multi-disciplinary training is to stimulate collaboration, including communication, situational awareness, problem solving, decision-making and teamwork.
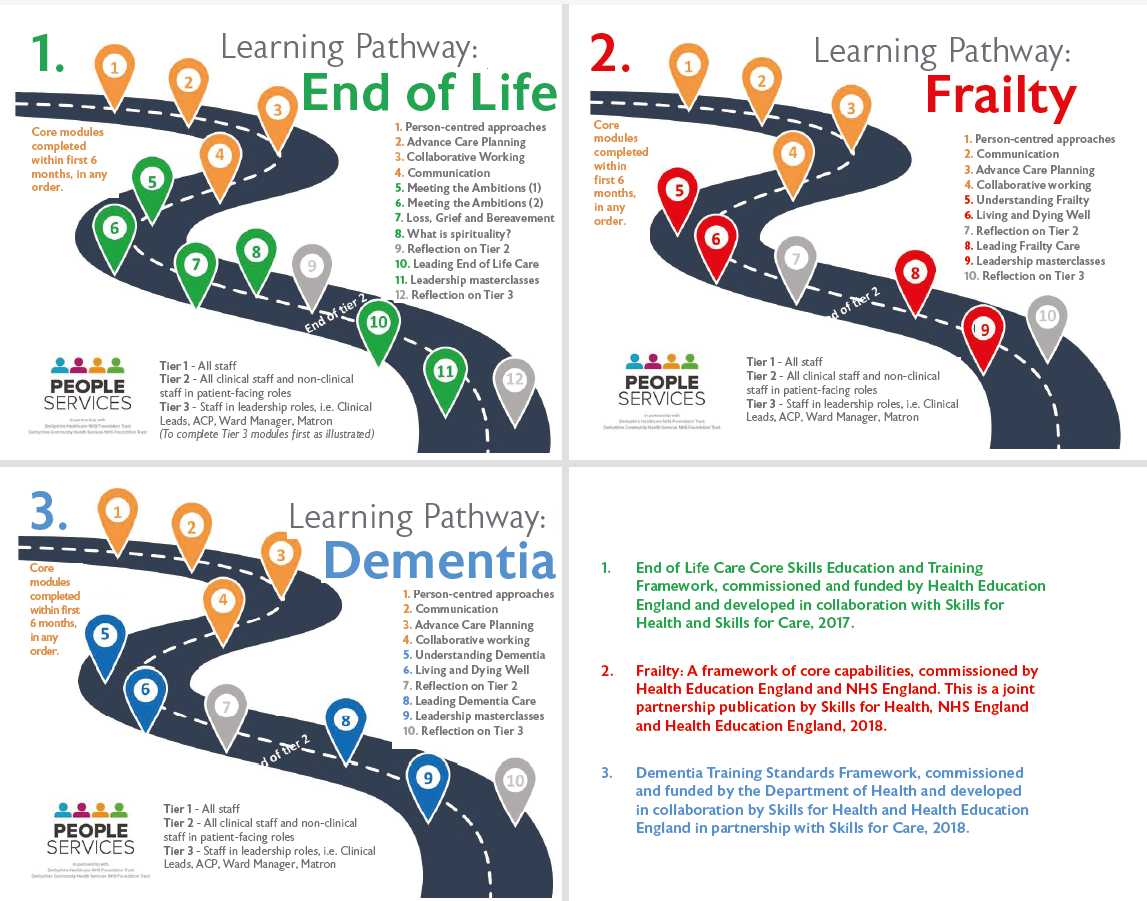
Comprehensive work was then undertaken to develop an integrated set of multidisciplinary learning pathways that incorporate the outcomes recommended within the three National Skills for Health frameworks (1,2 & 3) alongside identified local learning areas of needs and to be made available to staff from both Derbyshire Community Health Services NHS Foundation Trust and Derbyshire Healthcare NHS Foundation Trust.
Collaboration is key to the learning pathways as experts from practice across Derbyshire come together to create engaging and interactive sessions that will motivate learners to take knowledge back to practice. Experts range from clinicians and leaders within services, to Consultants and experts from other local NHS Trusts, public sector services, hospices, charitable services, voluntary services (see Figure 1, below).
Most importantly the voice of ‘experts by experience’ were heard and included within the programme of learning.
The pathways (see Figure 2, above) include common core modules which then lead staff to go on to further specialist modules within their selected area, with an online discussion forum to support them along their learning journey.
Tier 2 modules (for all clinical staff and non-clinical in patient-facing roles) will be completed over a 12-month period allowing staff to reflect and apply to practice before moving on to the next step in their chosen pathway, and those moving on to Tier 3 (staff in leadership roles) will have a further six months to complete the ‘leader’ level of their chosen pathway.
The final session at both Tier 2 and Tier 3 is to attend a Reflection module to allow time to look back on their individual learning journey, reflective on new knowledge and create an action plan (Tier 2) or service improvement project (Tier 3) to take back to their practice area, with motivation to implement change and share learning with others.
The future vision is for this common learning pathway to be rolled out across all organisations and teams in the Joined up Care Derbyshire (JUcD) Sustainability & Transformation Partnership (STP).