Frailty is a transitional state of vulnerability to accumulated impairments in physical, mental or environmental wellbeing and leads to a heightened risk of functional decline and crisis following even small changes to the physical, mental or the social and environmental state. It can be thought of as a long-term condition, but is not static, and can be improved with appropriate interventions. Frailty is a common condition which becomes more prevalent with age. It is thought to affect 25-50% of people over 80, and about 10% of those over 60.
Frailty is not a normal part of ageing and patients who are becoming frail can be proactively identified, as it develops over a 5-15 year period. However, patients often present in crisis, without prior warning, to urgent or emergency care services with one of the frailty syndromes (falls, delirium, immobility, etc). The population aged 85 and over (i.e. the ‘oldest old’) is the fastest growing age group in the entire UK population, and represents 2.1% of the total population of the UK. By 2033, the number of people aged 85 and over living in the UK is projected to increase to 3.3 million. Of these, 1.9 million will be aged 85-89, 962,000 will be aged 90-94, 384,000 95-99 and 80,000 will be aged 100 or more, according to The Kings Fund.
Older people living with frailty are the highest users of health and social care services, and have the highest number of unplanned admissions to hospital. Daily average emergency admissions to English acute hospitals for the >65 age group doubled between 2005 and 2012 and could do the same again by 2020 if there are no viable alternatives. 80% of emergency admissions who stay for more than two weeks are patients aged over 65, and just over 30% are over 85 years old. If the findings from the January 2016 audit of 31 GP practices across North Derbyshire are representative of the total North Derbyshire registered population, then there are more than 32,500 older people - 8.3% - who are frail.
The effects of frailty can be mitigated if problems are identified early. However, those affected are not always reliably identified, or are only identified when advanced frailty has developed. This means opportunities are missed to support people more effectively, which in turn leads to poor patient experience and avoidable care costs.
Identifying people living with frailty can help improve outcomes both in relation to a specific intervention as well as with the long-term management of health needs. Simple assessments can be used to identify frailty but should be followed up by a more detailed clinical assessment where necessary.
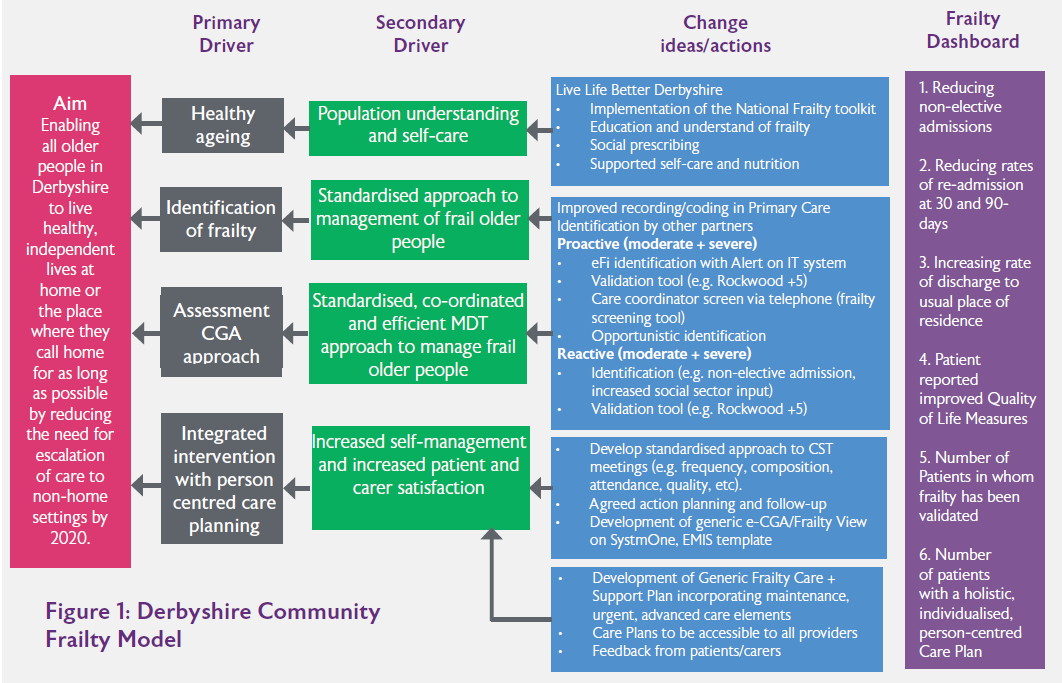
Joined-up Care Derbyshire (JuCD) Sustainability and Transformation Partnership’s (STP) mission is to improve population health outcomes for the people and communities of Derby and Derbsyhire with a vision for people to have the best start in life, to stay well, age well and die well. In support of the ageing well element, the Frailty Workstream of the STP has worked over the last four years to develop the Derbyshire Community Frailty Model (Figure 1). The workstream is a multi-professional, multi-agency group comprising providers, commissioners, Local Authority and voluntary sector representatives. Our goal is to enable all older people in Derbyshire to live healthy, independent lives at home or the place where they call home for as long as possible by reducing the need for escalation of care to non-home settings by 2020.
The Model comprises four key elements; Healthy Ageing, Frailty Identification, holistic assessment following CGA approach and integrated intervention with person centred care planning. The Frailty Dashboard within the model identifies a range of process and outcomes measures.
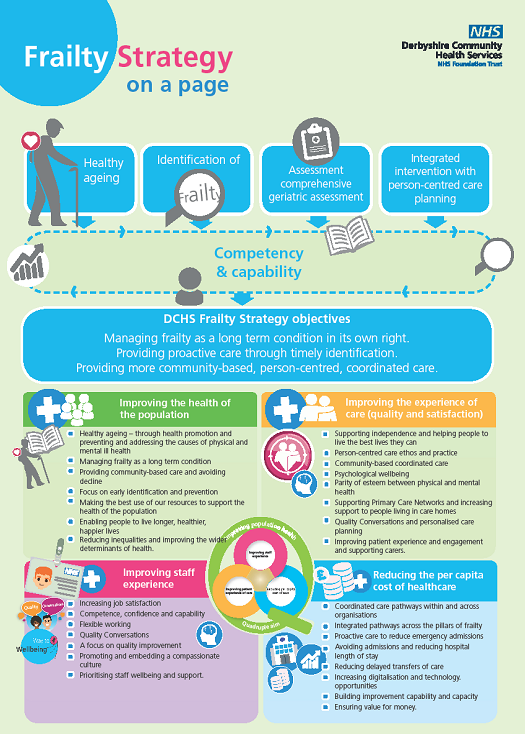
To support the delivery of the Derbyshire Frailty Model, the Derbyshire Community Health Services NHS Foundation Trust’s (DCHS) Frailty Strategy (see Figure 2) sets out our approach to the care of older people living with frailty. It has relevance and application to all people who are cared for within inpatient settings, community and General Practice. The strategy is informed by national guidance and is set in the wider context of JuCD STP. It articulates the Trust’s strategic aims in response to an ageing population and focuses on the ambition to treat older people as individuals who need person-centred, coordinated, community-based and integrated care rather than as a collection of multimorbidities.
We have also developed an End of Life Care Strategy and Dementia Strategy (in development), all three support our over-arching DCHS Clinical Strategy which is underpinned by the Quadruple Aim. The Quadruple Aim describes a vision of ‘simultaneously improving the health of the population, enhancing the experience and outcomes of the patient, and reducing the per capita cost of care for the benefit of communities; whilst ensuring staff have the best possible experience of work. The central premise of our Trust Clinical Strategy and its supporting strategies is Quality Improvement (QI), to this end, we have taken an approach that not only sets out our strategic intent but also clarifies detailed implementation plans to deliver high quality patient outcomes. Our strategic objectives are to manage frailty as a long term condition in its own right; provide pro-active care through timely identification and deliver more community based, person centred, coordinated care.
Workforce implications
There was recognition that there were quality, clinical, business and operational ramifications to the frailty agenda and these will need to be worked through and articulated within a comprehensive framework. Consideration was given to raising awareness and workforce training to meet the demands of a changing population profile (ageing and multi-morbidity) as well as wider system priorities.
Against this backdrop, the decision was made to create a Specialist Lead Trainer post, this coincided with Skills for Health publication of the Frailty Core Capabilities Framework. The brief was to map the dementia, end of life and frailty core capabilities frameworks and develop a training programme which prepared staff for the increasing acuity, complexity and dependency amongst older people living with frailty in our local system and work towards meeting our ‘Quadruple Aim’.