ForewordThe British Geriatrics Society (BGS) hosted an event in London on 12 September 2023 on ideas and practice around a minimum dataset for care homes. The BGS is a membership organisation of clinicians supporting older people and we wanted to use our network to bring health and social care practitioners together with academics, system leaders and policymakers. The task was to consider together how data could be better used to deliver the best possible care in UK care homes and domiciliary care. Our event brought together high-level stakeholders in health and social care across the four UK nations to share insights from the National Institute of Health Research DACHA study and from interRAI as well as from other studies using social care data. It enabled us to learn from the accumulated experience of research and data teams and to reflect on the “state of the art” in minimum datasets.
This policy report has been compiled from the presentations made at the event and the rich and constructive debate that followed. The COVID-19 pandemic has given new impetus to transforming how social care data is collected, shared and used. Our event demonstrated that there is a genuine appetite across the health and care sector to support those providing, receiving and commissioning care through better use of data. But this must be focused on the priorities of those living in care homes or receiving social care at home and of those supporting them.
In this report we make 12 recommendations for the effective implementation and delivery of a national minimum dataset that we believe policy-makers and regulators should consider. We look forward to working collaboratively to support efforts to improve care through better data.
Professor Adam Gordon
BGS President
|
1. Overview
The COVID-19 pandemic exposed the lack of visibility of people living in care homes in the UK. As infections spread, government policy action was hampered by a lack of basic information around the size and demographics of the care home population, the flow of people being admitted into or discharged from care home settings, and care home length of stay and life expectancy.1 This knowledge gap cost lives. At the heart of the problem: an absence of aggregated, accessible and standardised data.2 While several different bodies collect information on people in care homes – NHS trusts, local authorities, government agencies, researchers and care providers – there is no national, systematic approach or cross-sector coordination for how data is captured, shared and used to optimise social care.
2. Our 12 recommendations
We make 12 interdependent recommendations for the effective implementation and delivery of a national minimum dataset that policy and decision makers should consider in combination. They are grouped together under eight themes and expanded upon in section 6 of this briefing.
Recommendation 1
To ensure a national minimum dataset is genuinely a resource for better care, its format, content and method of implementation should be co-produced with the two stakeholder groups who are pivotal to its success: residents and their families, and care providers, comprising care home managers and frontline staff.
Recommendation 2
We need a sector-wide conversation around the data that does and does not need to be known by different stakeholders. This will help to negotiate and manage expectations for what data can be accessed, and by whom. A minimum dataset can be the basis for shared decision-making between commissioners, regulators and providers of services to older people living and dying in care homes.
Recommendation 3
The creation of a minimum dataset for care homes should prioritise the integration of a harmonised set of quality of life and quality of care indicators that are tailored to older adults with needs that cannot be met at home.
Recommendation 4
Data capture for a minimum dataset must not primarily be seen by care homes as a process for collating residents’ information for external users. A priority is to ensure care homes can easily derive actionable intelligence and insights from the data and use it to compare their home with the national picture.
Recommendation 5
An independent third party should be created to collect, hold, aggregate and disseminate the minimum dataset using a collaborative governance structure in which all parties agree on how their data is used.
Recommendation 6
Investment in a data-informed system for health care and social care can take us on a journey towards greater equity between the two. Government must seize the opportunity to use a minimum dataset for care homes to transform our understanding of the needs of a highly vulnerable population and engender greater respect for the contribution that care homes make to society.
Recommendation 7
A sustained approach to piloting a minimum dataset in care homes and gathering feedback from care staff and providers would support the sector in managing requests for information and in agreeing where changes are proportionate and necessary.
Recommendation 8
Detailed consideration should be given to how the linking of different information sources can maximise the value of a minimum dataset for care homes without putting individuals’ privacy at risk, and to communicating to the public how the data is used.
Recommendation 9
Time and resource should be invested in guaranteeing a high level of interoperability between the minimum dataset for care homes and existing software systems to facilitate effective data sharing across health care and social care services.
Recommendation 10
Government funding of dedicated in-home data coordinators to support the implementation of new data systems in Canada gives a strong flavour of the level of investment required to introduce a minimum dataset to the UK. The importance – and cost – of such roles should not be ignored.
Recommendation 11
A programme of research should be carried out into how new Artificial Intelligence capabilities can be harnessed safely and ethically to extract optimum value out of linked social care data.
Recommendation 12
To establish the foundations of a minimum dataset in the UK, we should combine valuable learning from the DACHA study, evidence of the analytic power of data instruments like interRAI that have been adopted in other countries, and the lived experience of those working in our care sector.
3. Policy landscape
Emergency measures introduced in response to the spread of COVID-19 allowed the UK Government to collect new data from social care providers to inform urgent policy action.
Having seen the resulting benefits of better data sharing, policymakers have since accelerated the adoption of data and digital technologies for social care. In Care Data Matters,5 published in February 2023, the UK Government set out its ‘roadmap for better data for adult social care’ in England. It has four overarching aims:
- Better joined-up care for individuals. Giving people who are receiving care the confidence that care providers have access to the right information, at the right time, to meet their needs.
- More staff time to care. Creating a data infrastructure to provide timely, accurate and accessible information that frees up staff time to focus on providing high quality, personalised care.
- Greater understanding of people’s care journeys. Using data to support integration across local health and care systems, by allowing health and care providers to share information and monitor quality and continuity of care.
- Better management of the health and care system. Ensuring that data underpins evidence-based decision making to improve care and enables transparency and accountability at every level.
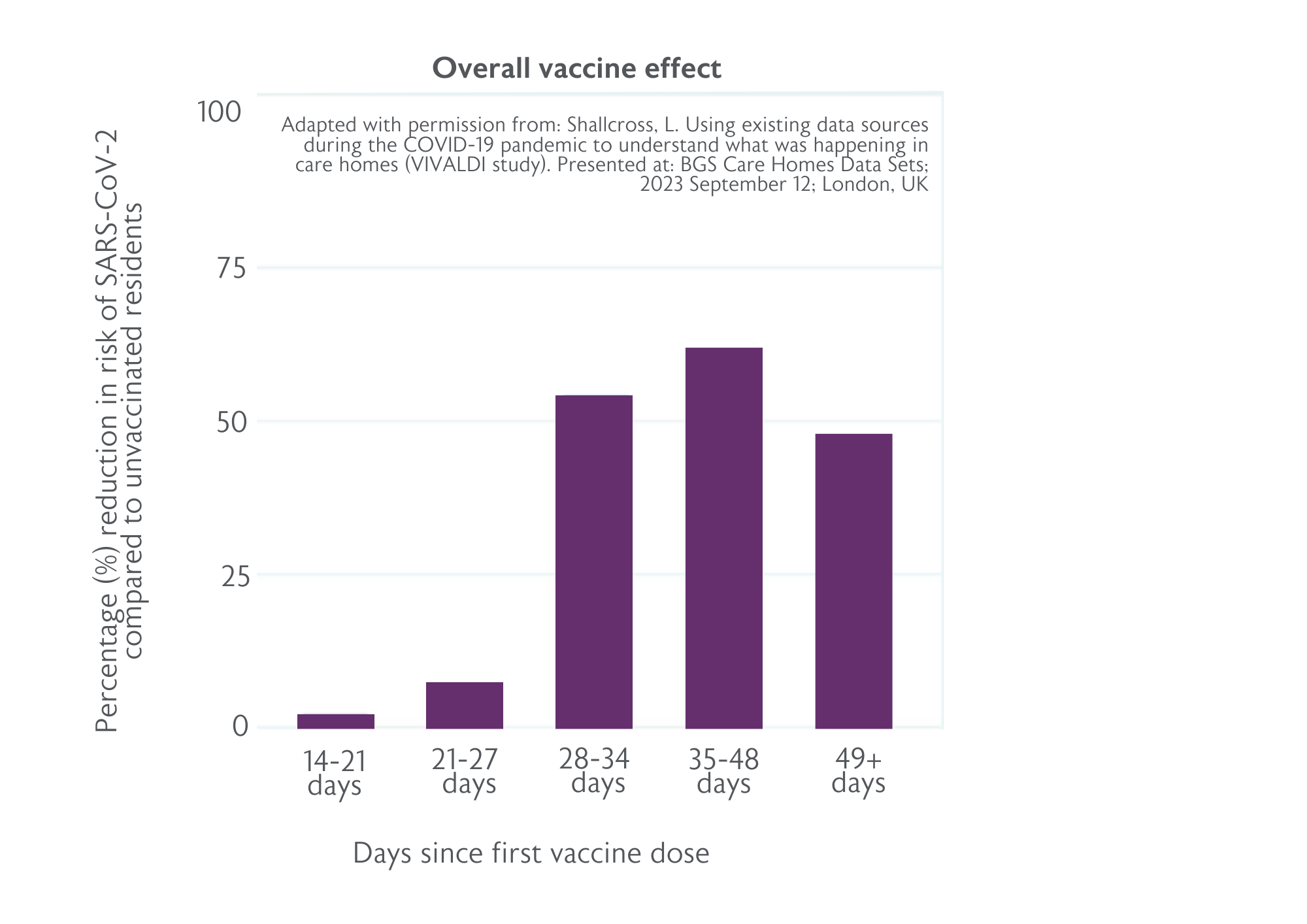
Progress is steady. About half of Care Quality Commission (CQC) registered providers in England are using Digital Social Care Records (DSCRs); the target is for 80% to have access to DSCRs by March 2024.5 There are 50 national social care data collections, including recent innovations like the Capacity Tracker, which collects real-time data on care home vacancies. Local authorities and providers are carrying out multiple regional data collections to support quality and risk monitoring and to identify areas for improvement. Beyond England, there is consensus among governments around the need for improved data collection in care homes. The Welsh Government published its Digital and data strategy for health and social care in Wales7 in July 2023, while data is a core component of Scotland’s My Health, My Care, My Home framework8 for adults living in care homes. But in this changing landscape, there are limitations that only a collaborative and systematic approach can address (see Figure 1).
As part of its plan to overcome these barriers, DHSC is developing a national operating minimum dataset to streamline how data is collected from care homes in England. To enable providers to record and access standardised information for care plans, the minimum dataset will establish a list of required fields that DSCRs must capture. DHSC intends to begin piloting a subset of this minimum dataset in 2024, with a long term aim of having data collection in place for the whole sector by 2028.5
4. Challenges facing the care home sector
The unique complexity of the UK care home sector presents multiple challenges to the harmonisation and sharing of resident data. Understanding this wider context is key to crafting a pathway towards a minimum dataset that offers genuine benefits to the whole sector.
Divided from the NHS, it is a heterogenous, independent sector comprising approximately 11,000 care homes operated by 5,000 different providers under a diverse range of business models, with some owned by ‘for-profit’ companies or individuals, and others operated by local authorities or charities.9 Homes vary in size from fewer than 10 residents to more than 100 and the sector has a large number of small operators. In England 75% of care home providers own just one home and these homes account for 38% of care home beds, according to the National Audit Office.10 It is a similar scenario in Scotland, where the Care Inspectorate estimates that 36% of care home beds are provided by small operators.11 Funding of care also varies widely. Nearly half of the UK care home population of 400,000 fund their own care or make top-up payments to increase their choice of care.9 Care delivery is spread across a multi-faceted mix of health and care services: care home staff, on-site registered nurses, NHS community nursing teams, GPs and specialist medical care.
This large, diverse and fragmented network of independent providers and caregivers differs vastly from countries where long-term care is more centralised. It highlights the importance of co-production in the creation of a shared minimum dataset, where care providers have as much influence as policymakers, regulators and researchers over its content and structure – and how it is operationalised. In doing so, this work can address inequitable access to resources across care homes and providers. Many care homes are at the beginning of working towards having the digital infrastructure (e.g. reliable Wi-Fi access, devices, digital records) and staff IT skills required for a data-driven transformation of long-term care.
A sector-wide lack of consistency around access to, and control over, data is another obstacle to success – as well as a key motivating factor for a shared dataset. While access to anonymised NHS data is managed through a formalised, national infrastructure, there is no systematic approach to governance of care home data, which is held by a mixture of private companies, regulators and health and social care providers.4 This creates a frustrating scenario where the NHS and local authorities hold various data about people living in care homes that is often inaccessible to care home staff, and data collected within care homes goes unseen by external health and care staff supporting residents.
Care homes receive multiple, overlapping data requests in different formats from a wide range of external agencies. However, once these requests are met, care homes rarely see how the data is used. This speaks to a fundamental issue: if statutory data collection imposes a significant administrative burden without providing any demonstrable benefits to those caring for people in care homes, the quality and usability of submitted data will fall. It will also take its toll on workforce wellbeing and morale. A survey of BGS members last year revealed the extent of the workload pressures experienced by health and social care professionals and the lasting impact of the COVID-19 pandemic.12 Therefore, the introduction of a minimum dataset needs to be intuitive and incorporated into a care home’s workflow. Staff must be able to see data capture, not as an administrative requirement, but as a tool that supports them to drive change and make a positive contribution to care.
5. Data in action: enhancing frontline care in care homes
Using data to improve and save lives in care homes
During the early stages of the pandemic, people living in care homes were more likely to be admitted to hospital or to die from COVID-19, compared to the general population. The VIVALDI study13 was set up in May 2020 to understand what was happening in care homes and address fundamental data gaps: how many people living and working in care homes were infected with COVID-19, and how many had been infected in the past? To inform urgent policy responses, this government-funded study, led by University College London, also sought to answer the question: Why are some homes getting large outbreaks and others are not?
Around 350 care homes had taken part in the study by March 2023. Data from more than 60,000 residents and staff was combined with serial blood sampling. The study explored how long antibody response to infection and vaccination lasts, and the extent to which this prevents re-infection. Antibody testing was linked to national datasets on PCR testing, vaccination, hospital admissions and deaths.
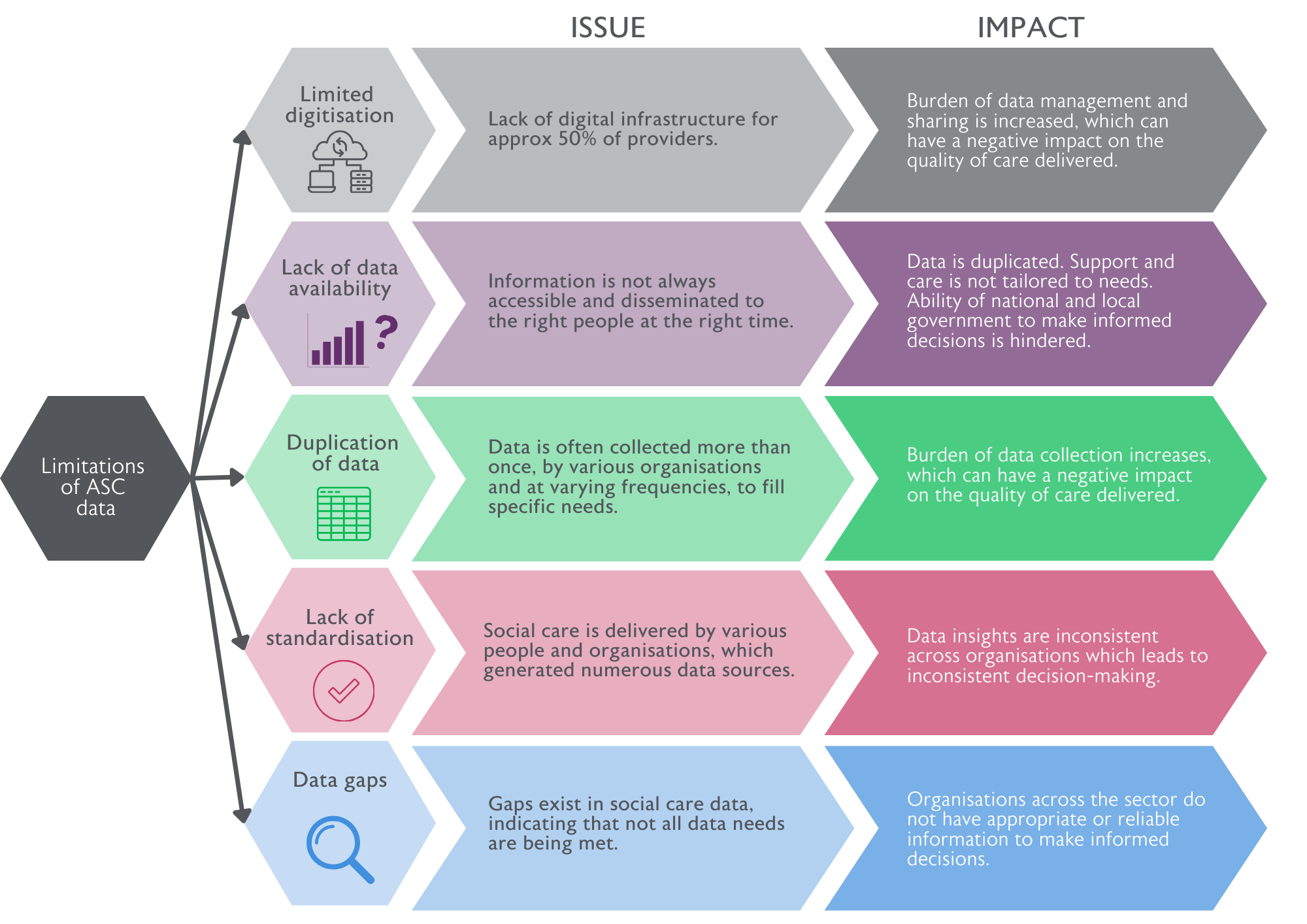
The VIVALDI study’s findings14 included:
- Staff were more likely to infect residents than vice versa.
- Care homes not paying full sick pay were more likely to have infections in staff and residents.
- Care homes where staff frequently worked across sites were more likely to have infections in staff.
- There was a 62% reduction in the risk of infection 35 days after a first vaccine dose (see Figure 2). From December 2020 to March 2021, the risk of infection for a typical unvaccinated resident was 5.8%; this fell to 2.3% after one vaccine dose.
These outcomes informed the following policy developments:
- Focusing limited COVID-19 testing capacity on staff not residents.
- Funding staff sickness pay through the infection control fund.
- Reducing movement of care home staff across sites.
- Identifying vaccine effectiveness among residents and staff and the need for boosters.
VIVALDI is evolving into a long-term programme of research and sentinel surveillance in care homes, under the continued leadership of Professor Laura Shallcross MBE (her MBE was awarded for this work), and in partnership with Care England and the Outstanding Society. Co-produced with care providers, residents and relatives, it aims to create a positive legacy from the pandemic by reducing the risk of a broader range of common infections and avoiding hospital admissions among care home residents.
Shallcross believes a better use of data can help level the imbalance between the NHS and the social care sector, bringing more parity between how they are perceived, and the resource given to them. With an emphasis on linking national and local datasets, the study aims to utilise existing data sources, keeping the input required from care homes to a minimum. For Shallcross, this sends a crucial message to the care home sector: data is about empowering you, not regulating you.
If we can do this kind of work during a pandemic, imagine what could be achieved if we adopted the same approach for other common infections, like flu or norovirus. We want to challenge the view that infections and outbreaks are simply an inevitable part of living in a care home, by delivering research and surveillance that tackles all kinds of infections.”
- Professor Laura Shallcross MBE
Developing and testing a minimum dataset in care homes in England
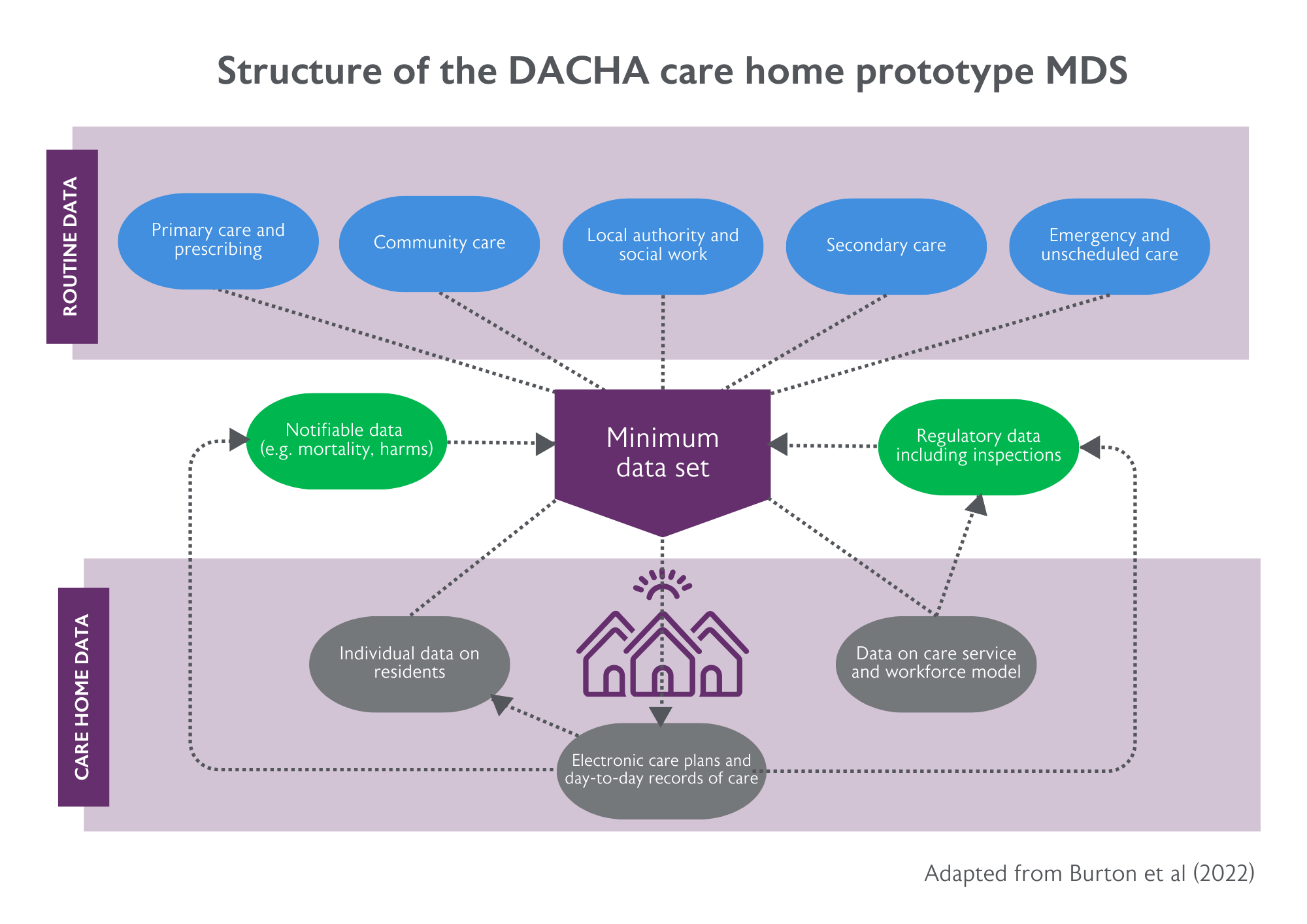
The DACHA study (Developing resources And minimum dataset for Care Homes’ Adoption) has two main aims: firstly, to establish what data need to be in place to support research, service development and uptake of innovation in care homes; and secondly, to synthesise existing evidence and data sources with care home generated resident data to deliver an agreed dataset (a minimum dataset) that is usable and authoritative for different user groups.
DACHA involves nine UK universities, the National Care Forum and the Health Foundation, and is funded by the National Institute for Health and Care Research. Led by University of Hertfordshire’s Professor Claire Goodman, the study grew out of research that demonstrated the importance of structuring support for care homes around the needs of residents – and is designed to address a very real risk that quality improvement initiatives, like data sharing, are developed without fully consulting the people receiving and giving care in care homes.15
To create its minimum dataset, the DACHA team carried out a national survey of 273 providers representing 5,000 care homes to explore what, how and why care home resident data is being collected, stored and shared. These findings were combined with outcomes from consultations with social care sector groups, reviews of clinical standards for health and care records, and content of minimum datasets used in other countries.16
They found that care homes already collect, use and share a vast amount of data on the health, care and support needs, the preferences and the daily activities of individual residents. However, there was a clear bias in the data towards health outcome measures and responding to external demands (e.g. regulatory oversight), but insufficient, unstandardised data on quality of life and social care measures. Based on these conclusions, DACHA researchers structured their prototype minimum dataset for care homes (see Figure 3) around refining, rather than reinventing, existing data, and around prioritising new data on social care outcomes.
Time spent collecting new or additional data is time not spent delivering care and has a cost. We need to keep the ‘minimum’ in the Minimum Dataset.”
- The DACHA study team
The DACHA team piloted this prototype minimum dataset in 45 care homes across three Integrated Care Systems. On top of data already held in DSCRs (e.g. resident demographics and needs, length of care home stay, diagnoses, medication), the team incorporated new measures on cognition, delirium, activities of daily living and quality of life (QoL). The latter comprised four specific measures: QoL for older people, social care-related QoL, health-related QoL and dementia-specific QoL.
Early findings indicate:
- It is feasible to refine and adapt existing methods of data capture and use DSCRs to extract data from care homes for a minimum dataset.
- The minimum dataset is acceptable to staff. They completed the additional data variables (e.g. quality of life measures) and saw value in them as an asset for care, not as an administrative distraction. They recognised the potential to reduce the current data burden and simplify sharing data between different teams.
- There is only partial uptake if key people move or systems change, meaning that sustained investment in implementation across different stakeholder groups and systems of care is key to delivering meaningful engagement with care homes.
- Care homes are the data controllers, and software vendors are the data processors. Different software systems have different processes, which has implications for a national-level rollout.
- There are opportunities to work with existing software and data capture practices to harmonise data sources, support interoperability and, ultimately, achieve scalability.
DACHA data collection and interviews with care homes are continuing. One of the team’s next steps is to determine what the minimum dataset can and cannot achieve for different stakeholders – and what it is reasonable to ask of care homes. At the heart of the approach is the need to minimise the burden on care homes by excluding data that is of little importance or value. As Goodman says: “Data should be seen as a tool, not a comfort blanket.”
DACHA-DOM: A minimum dataset for home careA study within a study, DACHA-DOM17 is exploring the feasibility of developing a minimum dataset for home care – a paid-for service that enables almost one million people with physical, mental and/or cognitive impairments to live and receive direct support at home. Home care is a highly fragmented sector: 10,800 organisations provide care (85% are private companies) with care staff among the lowest 20% of earners and requiring no minimum entry qualifications. Led by Professor Barbara Hanratty at Newcastle University, the study has surveyed home care providers, interviewed care recipients and families, and held focus groups with commissioners, academics and providers. Findings are at an early stage but so far, the DACHA-DOM team has been able to draw the following conclusions:
|
Using data to advance care practice: international perspectives
“Our use of data begins with the residents and their families.” This is the philosophy followed by Julie Weir, the CEO of New Brunswick Association of Nursing Homes in Canada, who has overseen a transformation in the use of resident data to guide decision-making across the association’s 74 private care homes.
Weir, herself a Registered Nurse, implemented the interRAI Long-Term Care Facilities (LTCF) Assessment System over one year in 2017. This is a standardised system that allows care providers to assess key domains of function, mental and physical health, social support and service use for those in nursing home institutional settings. The LTCF tool is one of several instruments developed, evaluated and made available by interRAI, an international, not-for-profit network of 140 researchers, clinicians and policymakers.
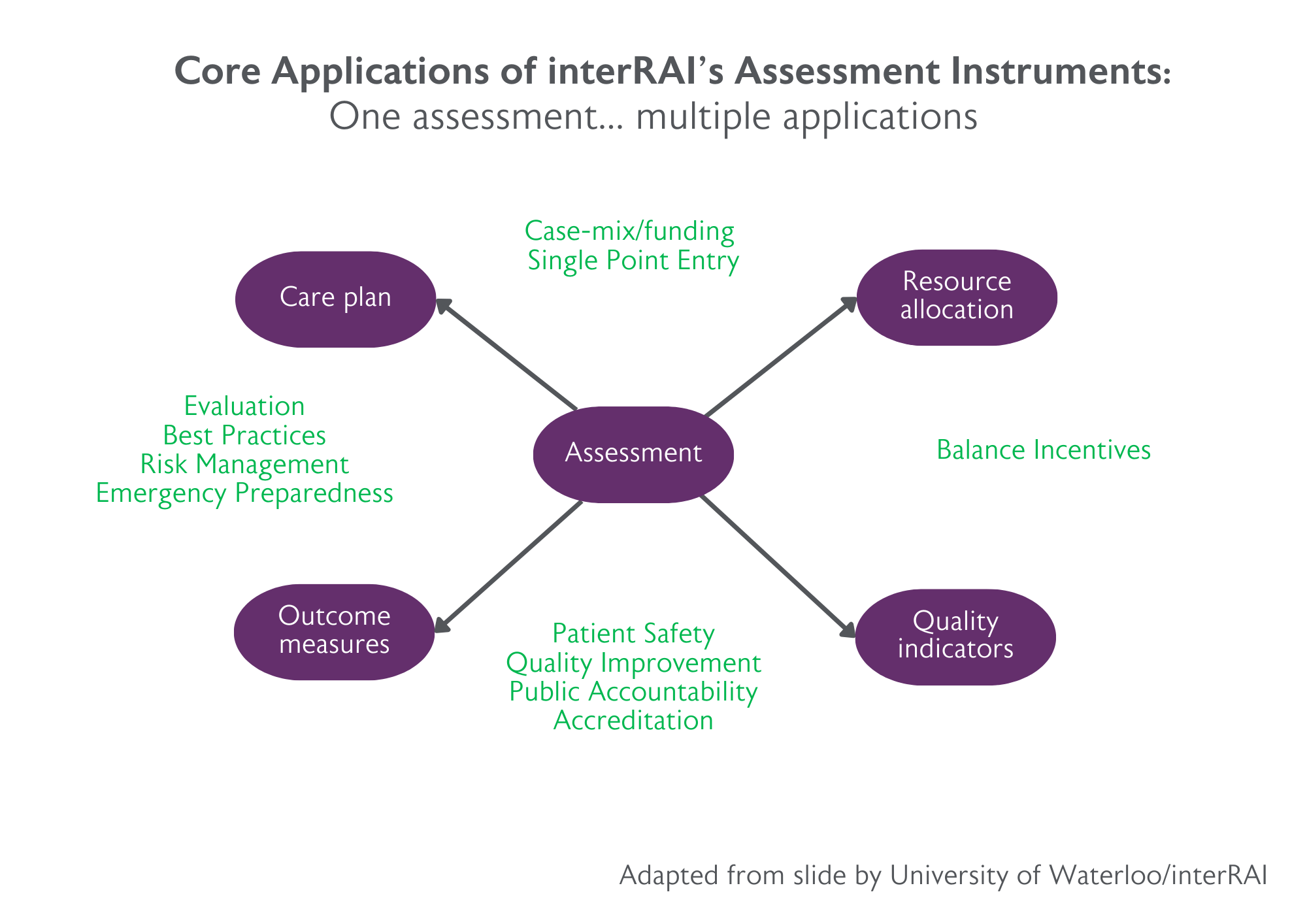
The interRAI instruments provide comprehensive assessments of the strengths, preferences and needs of vulnerable populations, and their use is mandated by governments in several countries, including in every one of Canada’s 14 health systems.18 Through a single assessment, the instruments are designed to inform care plans, outcome measures, resource allocation and quality indicators (see Figure 4).
For Weir, 2017 was a long 12 months. They were going from “nothing” to a comprehensive data capture system across an initial 10 homes, and it took time to get each home onside. “But once staff understood the benefits to themselves and the residents and their families, they were all in,” Weir said. Collaboration with residents and their families was crucial. Some families began to align their visits with the interRAI assessments. The data outcomes were validated during multidisciplinary care reviews and through discussions with residents’ families. For example, care staff showed families evidence of outcome scales changing and asked them if the data correlated with what they had noticed about their loved one.
We use the data to tell a story, validate the data based on conversations with residents and their families, and then use this information to improve care.”
- Julie Weir, CEO, New Brunswick Association of Nursing Homes
The newly available data guided both home and government decisions. Within the homes, they were able to better allocate staff resource, eliminate unnecessary routine paper-based assessments and compare Quality Indicators to identify specific interventions that would optimise care. At a government level, the interRAI assessments were integrated into annual inspections, used as evidence to justify funding need, and used for national-level benchmarking to identify homes at higher risk of adverse resident outcomes.
National benchmarking was “invaluable”, according to Weir. She felt their homes were offering high quality care but had not been able to evidence that with data. There was plenty of nervousness around how the media would report on the Quality Indicators. But when Weir saw the home-level results she was able to tell each home where to focus their energies to make improvements. And by the time outcome measures from 30 of their homes were reported nationally, they were shown to be performing above the national average on every indicator. “Proper risk adjustment of the data was really important. This allowed a 13-bed rural home to be compared accurately with a 200-plus bed city home,” said Weir.
Integral to the implementation of the interRAI system was investment by the provincial government in dedicated ‘RAI co-ordinators’ to capture and process the data from the assessments that each take 60-90 minutes and are required every 90 days. In the case of New Brunswick, one 200-bed nursing home employed a full-time funded Registered Nurse (with no specific data background).
The concept of quality reports can invoke a set of common reactions, according to John Hirdes, Professor of Applied Health Sciences at University of Waterloo, and Chair of the interRAI Network for Mental Health: “We often hear people say: my residents are different, we measure it in a different way, we can’t trust the data, we can’t change,” he said. “But risk adjustment considers factors like environment or case mix that may affect care quality; there are processes to standardise the data that are underpinned by training and statistical tools; and national benchmarking shows how other homes achieved meaningful change and keep pace with what is happening in the wider sector. Having worked through all that, we can then say: Let’s do something about it.”
interRAI Check-Up Self-Report: Getting to the rest of the storyFor Dr George Heckman, a practising geriatrician and Schlegel Research Chair in Geriatric Medicine at University of Waterloo, standards and stories both matter. Older populations are becoming ever more complex in their health needs, with increasing multimorbidity, polypharmacy and multi-ethnicity. In Heckman’s view, the more we can rely on standard, reliable and valid information to capture this complexity and deliver person-centred care, the more we can focus on a person’s narrative. Pursuing the former, Heckman has been carrying out research to validate the interRAI Check-Up Self-Report Instrument. This web-based tool has around 90 items that assess a person’s cognition and communication, mood and wellbeing, functional ability and various risk factors. In one study, Heckman and colleagues asked 184 older adults and their families, from diverse backgrounds in Canada, to complete the check-up themselves. The findings confirmed validity, reliability, acceptability and feasibility, with each self-report taking 28 minutes on average.19 The tool facilitates a more focused and complete care assessment and frees up valuable time to hear a person’s story, Heckman says. “I can see what’s going on and I can start focusing on what matters to them … To engage a person, you need to know who they are and what motivates them, but in the traditional approach you spend so much time collecting data on function, you never get to that,” he said. |
6. Ensuring a Minimum Dataset benefits care homes and their residents
This section sets out eight themes that address potential barriers to the successful implementation of a national minimum dataset in the UK and provides recommendations for how they can be overcome.
A shared understanding of purpose
The prospect of a standardised, collective dataset that can empower and support people living and working in care homes is compelling. But first, the sector needs to develop a common understanding of what a minimum dataset for long-term care should look like and why we want it.
Data content cannot prioritise the interests of some groups over others, for example regulators over residents. Rather, it should form the basis of a shared language that unites multiple stakeholders, and it must meet a range of complementary yet distinctive needs. In developing this shared understanding, it will be important to be clear on what a minimum dataset can and cannot do. For example, it will not replace an individual’s structured care plan (sharing such highly personal information would be unacceptable) but will be compatible with it. It will be much more dynamic than a compliance tool or an enhanced health record with some social care data added to it.
For residents and their families, a minimum dataset will identify how individuals’ needs are changing over time in the context of the home they are living in, informing interventions that improve their quality of life and experience of care. For care homes and their staff, it will provide actionable insights to optimise the care they give, monitor the effectiveness of in-home strategies and benchmark themselves against other care homes. For regulatory bodies, integrated care systems and national and local government, it will guide commissioning, policy and planning, and quality improvement. For membership bodies, it will inform policy development, lobbying and campaigning. For academia, it will provide new research insights and underpin epidemiological studies looking at population changes over time. And for the wider public, it will inform their choice of care when they need it.
| Recommendation 1: To ensure a national minimum dataset is genuinely a resource for better care, its format, content and method of implementation should be co-produced with the two stakeholder groups who are pivotal to its success: residents and their families, and care providers, comprising care home managers and frontline staff. |
| Recommendation 2: We need a sector-wide conversation around the data that does and does not need to be known by different stakeholders. This will help to negotiate and manage expectations for what data can be accessed, and by whom. A minimum dataset can be the basis for shared decision making between commissioners, regulators and providers of services to older people living and dying in care homes. |
Prioritising data that matters most to those receiving care
The success of a minimum dataset – data that is of high quality, complete and usable – rests on the ability of staff who are collecting it to see, quickly, its benefits, both for their own work and their residents’ health and wellbeing.
To truly deliver person-centred care, we need longitudinal data that moves beyond a narrow reliance on traditional health-oriented measures, towards a well-rounded picture of a person’s quality of life. This will require agreement over the integration of a set of indicators that capture mood, cognition, communication, relationships, loneliness and participation. In doing so, care providers can identify some of the more subtle, long-term changes in their residents’ status, triggering an awareness that adjustments to care are required.
|
Recommendation 3: The creation of a minimum dataset for care homes should prioritise the integration of a harmonised set of quality of life and quality of care indicators that are tailored to older adults with needs that cannot be met at home. |
Ownership, governance and access
Membership bodies like the National Care Forum (NCF), a leading voice for not-for-profit organisations in the care and support sector, view the design of a minimum dataset as a shared endeavour to improve care. They report enthusiasm among their members for valuable national benchmarking based on evidence that the sector can use together to support innovation, as opposed to it being carried out within an environment of compliance. As the NCF has said: “The power of data for social care is enormous, but it needs to be in our hands.”
It is crucial to support the ownership and use of the data within care homes and providers. What care homes are missing is an understanding of how data they collate and submit to external users is being used by different organisations. This is a demotivator for staff, hindering the capture and supply of high-quality data. But if homes are given access to intuitive data dashboards that clearly display trends over time, staff will see how changes to practice feed into quality improvements over the long term.
Care homes are people’s homes. It is of utmost importance, then, to protect the privacy of residents and avoid identifying individuals in secondary data uses. We need a sustainable, robust mechanism to anonymise data and impose strict access controls – a system of governance that can rise to the challenge of bringing together data held by a mixture of private companies, public institutions and not-for-profit organisations. Another key issue is the management of commercially sensitive data about the functioning of the sector. This is about striking a balance between public interest and an organisation’s ability to provide care services as workable businesses. This is likely to require the demarcation of clear boundaries between data collected for regulatory purposes, benchmarking data, and data that can be used by care homes themselves.
|
Recommendation 4: Data capture for a minimum dataset cannot be seen by care homes as a process for collating information for external users. A priority is to ensure care homes can easily derive actionable intelligence and insights from the data and use it to compare their home with the national picture. |
| Recommendation 5: An independent third party should be created to collect, hold, aggregate and disseminate the minimum dataset using a collaborative governance structure in which all parties agree on how their data is used. |
Trust and respect
There is strong feeling among BGS members around the need for parity of esteem between the social care and health care sectors. At our care data roundtable, one registered nurse in a care home expressed frustration at what she saw as a ‘punitive’ environment and a paternalistic approach from policymakers towards the social care sector.
They said: “We are done to, not respected. Sharing resident data requires a new foundation of trust and respect. But we are nowhere near a scenario where the care home sector is working alongside others to co-produce datasets.”
A principle of reciprocity is key. A drive to increase data collection is seen as a big ask of a system under strain. Many people working in care homes are worn down by a feeling that they are unable to deliver quality care. They are asking policymakers to be respectful of the pressures the workforce is under and ensure there is a two-way flow of information around data needs between the social care and health care sectors.
| Recommendation 6: Investment in a data-informed system for health and social care can take us on a journey towards greater equity between the two. Government must seize the opportunity to use a minimum dataset to transform our understanding of the needs of a highly vulnerable population and engender greater respect for the contribution that care homes make to society. |
Minimising the data burden
Rather than increasing administrative workloads, a minimum dataset is a chance to actively reduce duplicate reporting. Considerable time in care homes is spent providing data about their service and their residents to multiple external agencies, often involving the submission of the same data in different formats. This is time that could be used for care.
Collaborative working and ongoing engagement with care homes will ensure that the format, structure and timings of the requested data are aligned. Government will also need to be aware of the importance of a strategy to manage the transitional period between the current situation and more sophisticated data flows and platforms that will become the norm.
| Recommendation 7: A sustained approach to piloting a minimum dataset and gathering feedback from care homes and providers would support the sector in managing requests for information and in agreeing where changes are proportionate and necessary. |
Data linkages and interoperability
A minimum dataset for social care offers the enticing prospect of bringing together previously unlinked data sources to generate new insight into complex issues. It can unite information collated within a care home about individual residents, the workforce and the care service with regulatory data and external data about services supporting the home: primary, secondary and community care, emergency care and local authorities.
The Government’s Data Saves Lives Strategy has set the direction for how health and care data are integrated with other datasets to achieve a better understanding of the linkages and interdependencies between health care, social care, housing and other policy areas. The implementation of this strategy should emphasise continuity and consistency of approach towards information governance and accountability of those who agree priorities for analysis, and how this is presented publicly.
Similarly, software systems require linking up. Their interoperability is critical to facilitating data flows between systems operated by different software providers. Close integration between the minimum dataset and care home software is vital for efficient data collection and processing, and for making full use of the analytics tools already available.
| Recommendation 8: Detailed consideration should be given to how the linking of different information sources can maximise the value of a minimum dataset for care homes without putting individuals’ privacy at risk, and to communicating to the public how the data is used. |
| Recommendation 9: Time and resource should be invested in guaranteeing a high level of interoperability between a minimum dataset for care homes and existing software systems to facilitate effective data sharing across health care and social care services. |
Investment in digital infrastructure and training
Effective implementation of a minimum dataset – and equitable participation in it – requires significant government investment in digital infrastructure and training within care homes that goes beyond technical skills. Expectations around the speed of implementation also need to be realistic, considering the point from where many small operators are starting (e.g. a lack of reliable Wi-Fi access).
Necessary investment includes resource for the development of staff skills and a new ‘data culture’, where providers and frontline staff are equipped with knowledge in how to interpret and interrogate the data for the benefit of their own services and residents. There are opportunities to consider expanding new professional roles that can drive this culture change, for example care technologists. We can also learn from Canada here. As described in section 5, the provincial government in New Brunswick funds the training and employment of dedicated data coordinators, who are playing a crucial role in ensuring care homes in the province can complete mandated care assessments to a high standard.
Progress is being made around use of Artificial Intelligence technologies to maximise the value of NHS data. However, governments have said little about exploiting AI for the interrogation of data in social care. This feels like a missed opportunity.
| Recommendation 10: Government funding of dedicated in-home data coordinators to support the implementation of new data systems in Canada gives a strong flavour of the level of investment required to introduce a minimum dataset to the UK. The importance – and cost – of such roles should not be ignored. |
|
Recommendation 11: A programme of research should be carried out into how new Artificial Intelligence capabilities can be harnessed safely and ethically to extract optimum value out of linked social care data. |
Learning from the evidence and ‘what works’
In building a minimum dataset for care homes, we are not moving from a standing start. The DACHA study (section 5) has made substantial progress in developing and evaluating a prototype minimum dataset for the UK, involving care homes and providers from the outset, and sustaining this co-production approach throughout the programme of research.
The introduction of minimum datasets in health systems overseas also offer valuable learning opportunities. There are differences of opinion around the compatibility to the UK of instruments like interRAI used in nursing homes. The complexity of the social care system in the UK and access to medical care via General Practice makes it very different from more centralised health systems elsewhere in the world. On the other hand, interRAI instruments are in use in 35 countries, highlighting their versatility. What is clear is that there is plenty of available evidence to light the way forward for the UK.
| Recommendation 12: To establish the foundations of a minimum dataset in the UK, we should combine valuable learning from the DACHA study, evidence of the analytic power of data instruments like interRAI that have been adopted in other countries, and the lived experience of those working in our care sector. |
7. Conclusion
A few years ago, there was little impetus for a national conversation around better use of data in care homes. COVID-19 changed that. It taught us that we cannot hope to protect one of the most vulnerable groups in society without the high-quality data we need to understand them and guide decision making for their benefit.
Out of that tragedy has come a new opportunity: transforming how adult social care data is collected, shared and used, not only to increase the sector’s resilience at times of emergency, but also to increase and sustain older people’s access to more personalised, integrated care over the long term.
Our roundtable demonstrated a real appetite from across the health and care sector for a greater, smarter use of data to support those providing, receiving and commissioning care. But the caveats are clear. This must be data created by the sector, to empower the sector. We call on policymakers and regulators to follow our recommendations and ensure that new data systems are tailored to the priorities of those living in care homes and those supporting them, and underpinned by substantial investment to overcome barriers to their effective implementation.
References
Click to expand
- Burton J, Goodman C, Guthrie B, Gordon A, Hanratty B, Quinn T. Closing the UK care home data gap – methodological challenges and solutions. International Journal of Population Data Science. 2020; 5(4): 1391. doi: 10.23889/ijpds.v5i4.1391
- Hanratty B, Burton J, Goodman C, Gordon A, Spilsbury K. Covid-19 and lack of linked datasets for care homes. BMJ 2020; 369. https://doi.org/10.1136/bmj.m2463
- Data.CMS.gov, Centers for Medicare & Medicaid Services. Minimum Data Set Frequency. 2023. Available at: https://data.cms.gov/quality-of-care/minimum-data-set-frequency
- Burton J, Wolters A, Towers A, Jones L, Meyer J, Gordon A, Irvine L, Hanratty B, Spilsbury K, Peryer G, Rand S, Killett A, Akdur G, Allan S, Biswas P, Goodman C. Developing a minimum data set for older adult care homes in the UK: exploring the concept and defining early core principles. The Lancet Healthy Longevity, Volume 3, Issue 3, E186-E193, March 2022. https://doi.org/10.1016/S2666-7568(22)00010-1
- Department of Health and Social Care, Care data matters: a roadmap for better data for adult social care. 2023. Available at: https://www.gov.uk/government/publications/care-data-matters-a-roadmap-…
- DACHA: Developing research resources And minimum data set for Care Homes’ Adoption and use. Funded by National Institute for Health and Care Research. Available at: https://dachastudy.com/
- Welsh Government, Digital and data strategy for health and social care in Wales. 2023. Available at: https://www.gov.wales/digital-and-data-strategy-health-and-social-care-…
- Scottish Government, My Health, My Care, My Home – healthcare framework for adults living in care homes. 2022. Available at: https://www.gov.scot/publications/health-care-home-healthcare-framework…
- Mary Daly. COVID-19 and care homes in England: What happened and why? Social Policy Administration. Volume 54, Issue 7, 985-998, December 2020. https://onlinelibrary.wiley.com/doi/10.1111/spol.12645
- National Audit Office. The adult social care market in England. 2021. Available at: https://www.nao.org.uk/wp-content/uploads/2021/03/The-adult-social-care…
- British Geriatrics Society. Ambitions for change: improving healthcare in care homes. 2021. Available at: https://www.bgs.org.uk/sites/default/files/content/attachment/2021-08-0…
- British Geriatrics Society. Lessons from the COVID-19 pandemic. 2022. Available at: https://www.bgs.org.uk/LessonsFromCOVID
- VIVALDI care home study. Funded by the UK Health Security Agency. Available at: https://www.ucl.ac.uk/health-informatics/research/vivaldi-study and https://theoutstandingsociety.co.uk/case-study/vivaldi-care-home-study/
- Shrotri M, Krutikov M, Palmer T, Giddings R, Azmi B, Subbarao S, Fuller C, Irwin-Singer A, Davies D, Tut G, Bernal J, Moss P, Hayward A, Copas A, Shallcross L. Vaccine effectiveness of the first dose of ChAdOx1 nCoV-19 and BNT162b2 against SARS-CoV-2 infection in residents of long-term care facilities in England (VIVALDI): a prospective cohort study. The Lancet Infectious Diseases. Volume 21, Issue 11, 1529-1538, 2021. https://doi.org/10.1016/S1473-3099(21)00289-9
- Gordon A, Spilsbury K, Achterberg W, Adams R, Jones L, Goodman C. From Warkworth House to the 21st century care homes: progress marked by persistent challenges. Age and Ageing. Volume 51, Issue 7, July 2022, https://doi.org/10.1093/ageing/afac169
- Musa M, Akdur G, Brand S, Killett A, Spilsbury K, Peryer G, Burton J, Gordon A, Hanratty B, Towers A, Irvine L, Kelly S, Jones L, Meyer J, Goodman C. The uptake and use of a minimum data set (MDS) for older people living and dying in care homes: a realist review. BMC Geriatrics. 2022, Jan 7;22(1);33 doi: 10.1186/s12877-021-02705-w
- Developing a minimum data set for homecare (DACHA-DOM). Funded by National Institute for Health and Care Research. Available at: https://dachastudy.com/dacha-dom
- interRAI: a collaborative network of researchers and practitioners in over 35 countries. Available at: https://interrai.org/
- Iheme I, Hirdes J, Geffen L, Heckman G, Hogeveen S. Psychometric Properties, Feasibility, and Acceptability of the Self-Reported interRAI Check-Up Assessment. Journal of the American Medical Directors Association. 2022 Jan;23(1):117-121. doi: 10.1016/j.jamda.2021.06.008
Contributors
Click to expand
With thanks to the following individuals who contributed to this report:
- Dr Eileen Burns, National Specialty Advisor for Older People and Integrated Person-Centred Care at NHS England
- Professor Claire Goodman,* Professor of Health Care Research at the University of Hertfordshire and Adjunct Professor at the University of Technology of Sydney
- Professor Adam Gordon,* President of the British Geriatrics Society, Professor of the Care of Older People at the University of Nottingham, and Consultant Geriatrician at the University of Derby and Burton
- Sally Greenbrook, Policy Manager, British Geriatrics Society
- Professor Barbara Hanratty, Professor of Primary Care and Public Health at Newcastle University and Deputy Director of the NIHR Older People and Frailty Policy Research Unit
- Dr George Heckman, Associate Professor and Schegel Research Chair in Geriatric Medicine at the University of Waterloo, and Assistant Clinical Professor at McMaster University
- Professor John Hirdes, Professor of Applied Health Science at the University of Waterloo, and Fellow of the Canadian Academy of Health Science
- Liz Jones, Policy Director at the National Care Forum
- Sarah Mistry, Chief Executive, British Geriatrics Society
- Professor Laura Shallcross, Director of UCL Institute of Health Informatics and Professor of Public Health and Translational Data Science at UCL
- Professor Ann-Marie Towers, Professor of Social Care at the University of Kent
- Julie Weir, Chief Executive Officer, The New Brunswick Association of Nursing Homes
*Disclaimer: The DACHA study is funded by the National Institute for Health Research Health Service & Delivery Research programme (NIHR HS&DR project number NIHR127234) and supported by NIHR Applied Research Collaborations (East of England, East Midlands, Yorkshire and Humber, Northeast and Cumbria). Claire Goodman and Adam Gordon are NIHR Senior Investigators. The views and opinions expressed are those of the DACHA team and do not necessarily reflect those of the NIHR HS&DR, ARC, NIHR, NHS or the Department of Health and Social Care.