Jon Bennett is a Respiratory Consultant and Chair of the British Thoracic Society.
The novel Wuhan coronavirus, COVID-19, has been shown to affect every age group across the world. However, the severity with which it manifests, and the outcomes of the disease, appear to worsen with increasing age of the person infected.
We are now aware of the different phases of the disease with the initial flu like illness during the first 5 days or so followed by the potential for COVID-19 pneumonia between days 5 to 10. Once the symptoms of COVID-19 pneumonia appear, patients can deteriorate very quickly. The most dangerous aspect of the disease, which I have witnessed on my COVID ward, is that the primary COVID-19 pneumonia progresses very quickly in some patients, meaning patients move from low oxygen needs to extremely high requirements and/or Critical Care within hours. In these cases it is vitally important to be able to recognise the patient’s deteriorating condition, and to intervene swiftly and appropriately. Timing, at this point, can make all the difference to the patient’s trajectory.
Many of the patients that geriatricians look after will have pre-existing conditions and functional impairment, making them more at risk from the virus. COVID-19 has a significant mortality rate in older, co-morbid patients with the potential for these changes to occur rapidly, forcing us to change the way we practise medicine. Given the manner in which patients can deteriorate we are now expected to make crucial decisions regarding ceilings of treatment at the start of the patient’s hospital admission.
This can feel uncomfortable, and particularly so for those of us with older patients in our care. There are recommendations in place regarding assessment, with Clinical Frailty Scores being the core assessment tool, a topic also recently covered in the two blogs; Frailty and Lung disease: best practice and Frailty – busting a few myths about what it is and what it isn’t. Restricted visiting has also made communication and shared decision-making with patients and family members more difficult and stressful.
At the heart of this, we know that the median time for intubation and ventilation for a patient with COVID-19 is 10 days and many of these critical care patients require complex cardiovascular support, with some also requiring renal replacement therapy. We all know Critical Care is not a benign therapy, with survivors having the potential to suffer ongoing problems. It feels that one needs to be ‘fitter than usual’ to have a reasonable chance of surviving a critical care admission due to COVID-19 and therefore more than ever, we need to consider what options are suitable for our patients. Our compassion and ability to communicate these difficult messages have to be at the core of all that we do.
We are having to abandon, temporarily, many years of established, well-founded practice as being irrelevant for this new disease entity. With COVID-19 pneumonia, antibiotics have no/minimal role, the standard Community Acquired Pneumonia assessment and CURB65 score has no value, the stethoscope adds little to the assessment process except in patients with airways disease (ie asthma and COPD), and monitoring is done with oxygen saturation rather than blood gases (except in patients at risk of hypercapnic ventilatory failure). Clinicians do however need to have an understanding of oxygen delivery including Venturi, non-rebreather masks and Continuous Positive Airway Pressure systems as this, and fluid balance, is the core treatment option.
There are quick ways to catch up with the essential things you need to know now.
The British Thoracic Society (BTS), with the help of its members, is maintaining a page where it publishes freshly developed guidance and advice to deal with a range of respiratory diseases and techniques in patients affected by COVID-19. It ranges from COPD to Pulmonary Rehabilitation, and covers Non-Invasive Ventilation, Interstitial Lung Disease (ILD), and more.
If you are short of time and don’t know where to start, this is the best place to get up to speed with the respiratory information you really need. It’s regularly updated, so you can be sure you are always looking at the most recent content.
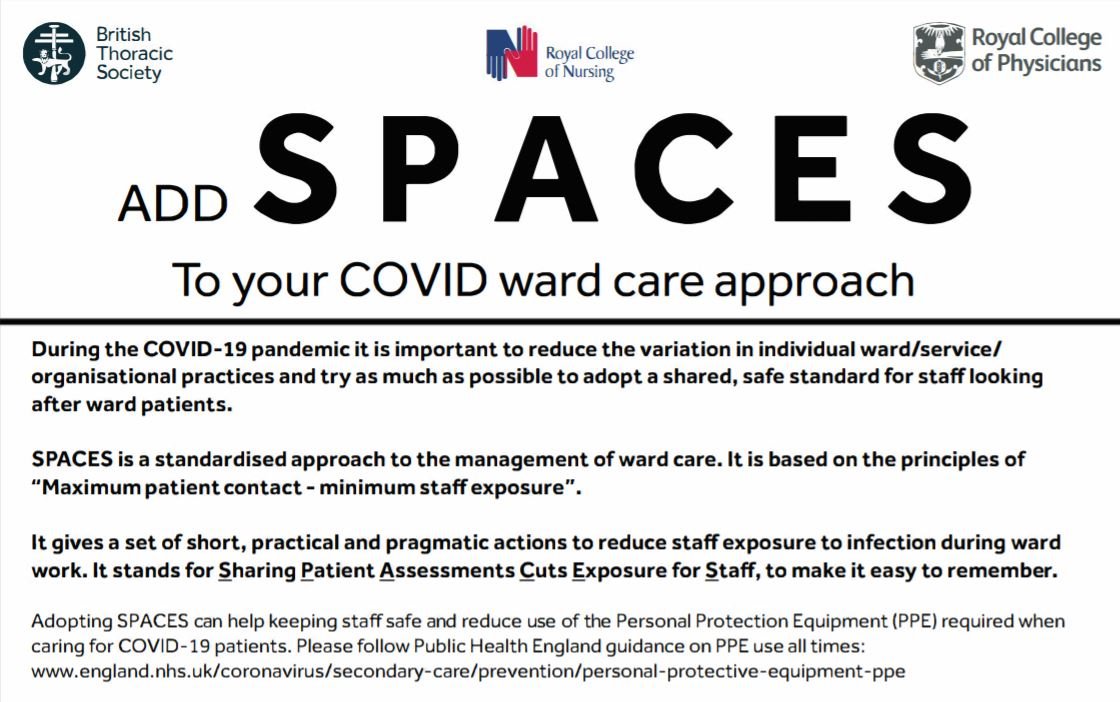
Staff safety remains an ongoing concern and we have tried to think about new ways of ward working, information on which is available on the BTS COVID-19 page. It is an alternative approach to ward care during this pandemic, concentrating on multi-professional working, maximising each staff-patient interaction and thereby reducing overall staff exposure to the virus and the reduced usage of already scarce PPE supplies. It can apply to any ward, not just in a respiratory department.
Sharing
Patients
Assessment
Cuts
Exposure for
Staff
It has been endorsed by the Royal College of Physicians, the Royal College of Nursing and we are expecting NHS England to put their stamp on it too shortly.
These are strange and stressful days. We will all make mistakes and feel overwhelmed at some point but, whenever this gets to you, remember that all of us are doing the best we humanly can.
Let’s all take care and stay safer with SPACES.