David Oliver is a Consultant Geriatrician in Berkshire and a visiting Professor in Medicine of Older People at City University, London. He is President Elect of the British Geriatrics Society.
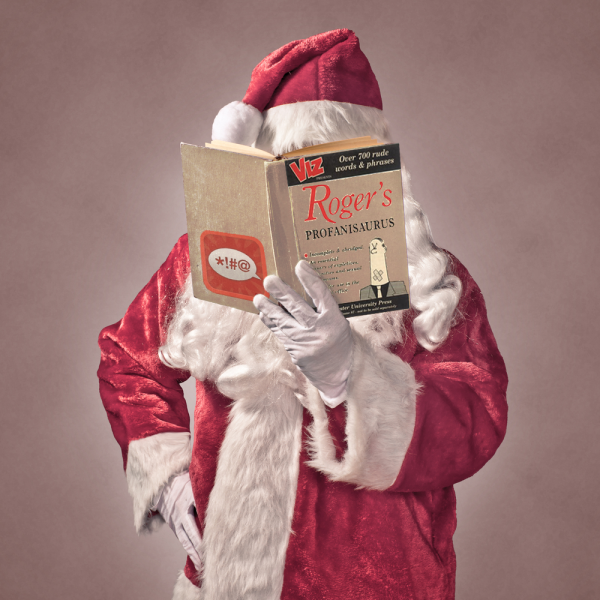
During the BGS Spring Meeting in Belfast, Prof Des O’Neill – probably the most cultured and literate geriatrician in our midst, asked many delegates, notebook in hand, for tips on enlightening books to further his thirst for broad knowledge. Earnest as ever, I suggested George Haidt’s “The Righteous Mind” and Ha-Joon Chang’s “23 Things They Don’t Tell You about Capitalism!”. Our then Hon. Sec., the redoubtable Dr Zoe Wyrko, mischievously and persistently tried to persuade Desmond that the book he really needed was “Roger Melly’s Profanisaurus” from Newcastle’s Booker-winning publishing house, Viz magazine. I did have a wry smile at the idea of the Amazon package being eagerly opened in Dublin the following week –contents taking pride of place in vertiginous O’Neill bookshelves. I also got to thinking, “sod Roger” – what about “Dave’s Profanisaurus of Geriatric Medicine?”. Though I don’t believe in censorship, we could list some terms that might result in an on the spot fine, a penance of extra fire safety training or a morning spent being the 15th member of the entourage following General Surgeons, P-Diddy style, round the wards.
I want to encourage my fellow BGS-ers to join in the fun and add their own “unutterables” but here is my start.
“Acopia”/”Acopic”. [sic] Whenever I see this term in patients’ notes I take the doctor aside for some gentle “re-education”. The thing I am proudest of writing is my 2008 essay in the JRSM Acopia and Social admission are not diagnoses. As Bytheway and Johnson stated, “ageism can range from well-meaning patronage to unambiguous vilification”. Giving some colleagues the benefit of the doubt, at best the “A” word means, “I have no training in dealing with frailty and no understanding that functional impairment usually comes with treatable diagnoses”, at worst, “older people are a just a bit crumbly, its their age, what did you expect?” or,“I can’t be bothered to try making a diagnosis”.
“Off legs ? Cause” comes under this broad umbrella. After my essay, two enterprising registrars, Drs Kee and Rippingale published an analysis in Age and Ageing of a series of cases of “acopia” – turns out it’s a dangerous diagnosis, encompassing for instance, cancer, severe sepsis, stroke & acute kidney injury. I still have medical colleagues saying to my geriatrician-face “I have an old boy for you, he is a bit acopic”. They do so, clearly unaware of the physical danger they have put themselves in.
“Social Admission” [See “Acopia” – above]. This is sometimes a variant on the theme. Readers, I kid you not, I have seen patients with two broken arms, one wrist fracture, spinal cord compression, sepsis and subdural labelled as “social admission” – not to mention those with severe dementia syndrome. In the case of the patients with fractures, I have been known to say, “so why didn’t you send them to the social worker instead of the fracture clinic then?”. An admission could only count as “social” in someone with no acute illness or injury, no recent change in function or cognition, whose carers have withdrawn and called 999, or perhaps someone with Dementia found wandering in the supermarket. And such people should, of course, not be admitted from the front door of the hospital as we can add no value to their care.
“Bed Blocker”. A couple of years back, when I was still the National Clinical Director for older people, I did 12 radio interviews back-to-back for the minister discussing the rise in “bed blockers”. I pointed out on every breakfast show that these were people, as entitled to care as any other citizen and that if they weren’t in hospital they would still be requiring publicly-funded care. Such terminology is depersonalising and adds to the narrative of older people being a threat to our services and a drain on resources – which is, of course, not true.
“The stroke in D4”. Ladies and gentlemen, this is a person….and someone’s mother, father or spouse. Someone with likes and dislikes, needs and wants, a life-history and deserving of respect as an individual. Reducing them to a number is profoundly disrespectful – think “prisoner 62”. And before you pull the data protection and confidentiality card, a BMJ survey of patients and public showed them to be intensely relaxed about their name being on display above the bed. Most patients expect professionals to share information about them with one another and we don’t conduct our board rounds using megaphones. Try stopping staff and saying “what’s that patient’s name?” and see if they always know.
“Mechanical Fall”. As all well-trained geriatricians know a fall in an older person generally results from a combination of activity, intrinsic risk factors such as gait, balance or eyesight, and external environmental ones. To be truly “mechanical” we need a fit person with no intrinsic factors slipping on the ice or a banana skin. Its just nonsense – stop it! And again, think about trying to make a diagnosis rather than “presenting complaint – fall; diagnosis – fall”. As Roger Melly would say “B****cks!”
“Failed OT assessment” and “Failed Discharge” One does not “fail” an OT assessment. The OT describes your ability to complete activities of daily living, contextualises this by describing premorbid abilities and then considers the support/equipment/rehab required to bridge the gap. I wish people would stop saying this. And as for “emergency readmissions” – they frequently occur in people for whom discharge was very carefully planned and supported. Guess what? Conditions relapse. People get new illnesses. People can panic. We need to accept some risk in helping older people return home.
Well, that’s my Mancunian ha’porth of profanities. Who else wants to join in the fun?