Date
Dr Premila Fade is a Consultant Geriatrician at Northwick Park Hospital, Co-Chair of the new BGS End Of Life Care Special Interest Group (SIG) and Co-Editor of the BGS guidance on End of Life Care in Frailty. She Tweets as @premzf.
The newly formed End of Life Care Special Interest Group (SIG) is proud to launch our online compendium of guidance on End of life Care in Frailty. The culmination of 18 months’ work, it is just the start of our collective effort to continue to improve end of life care for older people living with frailty. We had intended a big launch at the BGS Spring Meeting. As you know, this has been cancelled due to the pandemic, and hence this online launch.
With COVID-19 sadly taking so many lives, we feel that this guidance is even more urgently needed. We stand beside our social care colleagues, and with families and carers, in striving to provide the best possible care for older people living with uncertainty about their future. We know we cannot always prevent death, but we can improve quality of life and reduce the burden of futile medical intervention at its end. Now more than ever, it is important that advance care planning is seen not as a means of rationing healthcare, but as a way of easing suffering without wasting time, which is particularly precious towards the end of life.
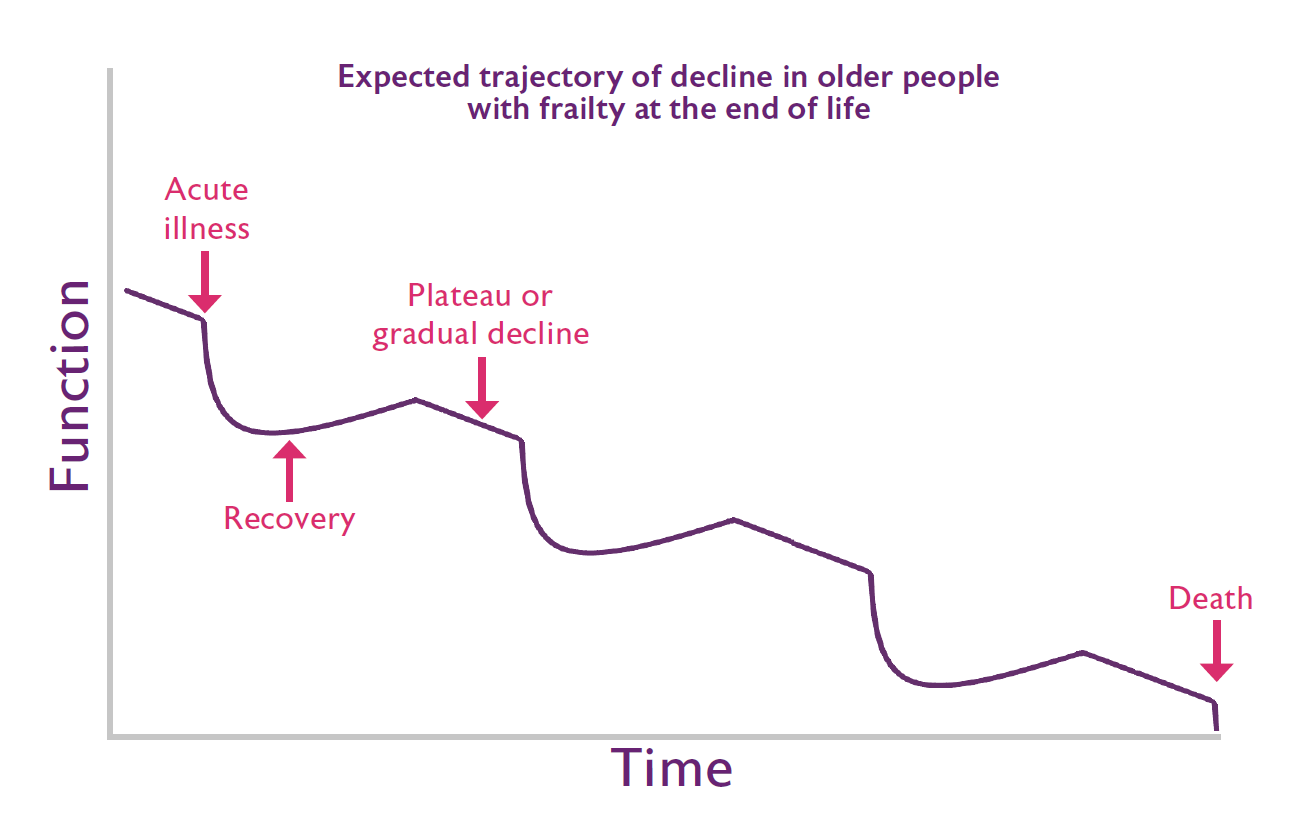
Some of you may be wondering why we need this guidance, or what is different about end of life care for people living with frailty. Geriatric medicine and palliative medicine have many shared values including our focus on multi-dimensional assessment and care, and person-centred decision making. However, there are also differences. Clinicians specialising in older people’s services work at the interface between disease-focused treatment and palliation, simultaneously planning for recovery and end of life. These dual priorities are of equal importance in our work, requiring us to move beyond the medical model of disease to a focus on enabling older people with frailty to live and die well.
We have published these guidelines on the BGS website to ensure they are easily accessible and can be updated as needed. This is a community effort. These guidelines are written by your peers: health and social care professionals passionate about providing the best possible care to older people living and dying with frailty. We know we haven’t included everything and that our practice is constantly being updated by new evidence and quality improvement. We therefore welcome your comments, particularly if you have suggestions about where the guidance can be expanded or improved to better help you, and in doing so, help your patients.
Category