About Geriatric Medicine
Providing healthcare to older adults is often extremely challenging. Patients often have multiple long-term conditions, and present to healthcare in atypical ways. Their care is defined by complexity. Doctors need to be highly competent communicators with knowledge of medical ethics, social care and palliative medicine. Most geriatricians are based in hospital and deal with acute medical illness but many geriatricians sub-specialise and do considerable work in clinic, the community and peripheral rehabilitation settings.
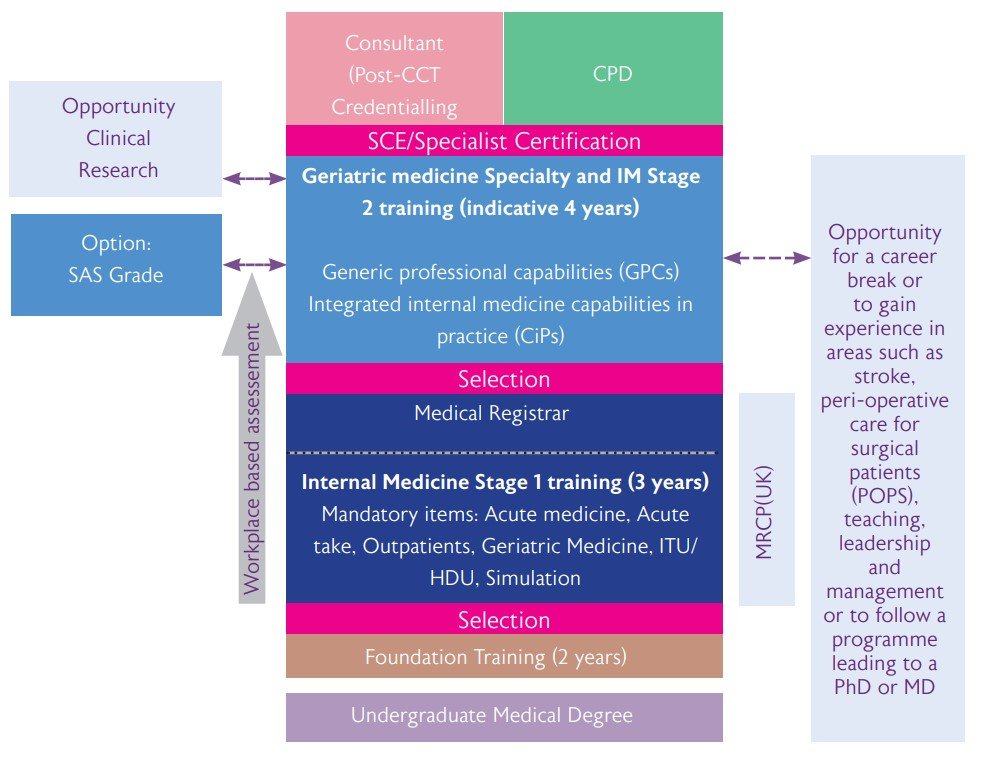
Academic gerontology is an exciting and expanding area. Research opportunities range from biogerontological research looking at interventions to modify or reverse the frailty trajectory, through to applied health services research considering how to care best for older people with complex conditions in a health and social care sector defined by constrained resources. Funding opportunities have expanded considerably within recent years and competitive Academic Clinical Fellowship and Lectureship posts in geriatric medicine are available in a number of world-leading centres based in the UK. International research collaborations around ageing are increasingly well developed and there are increased opportunities for academic geriatricians to travel as part of their work.
The attractions of Geriatric Medicine
- Geriatrics provides variety and challenge whilst being fun and rewarding
- Geriatric medicine is a combination of general and specialist practice
- It is practised in varied work settings, in hospital and the community, and has substantial scope for sub-specialisation
- There are many opportunities for research and teaching
- It incorporates collaboration with other specialties
- It involves teamwork with other healthcare professionals
- It requires collaboration with social services and private and voluntary sectors
- It has good career prospects, and geriatricians work in every acute trust in the UK. There is likely to be a job for you, wherever you want it
- There are opportunities for less than full time work
- It provides real rewards of making a difference to the patient and their family where others may have given up.
Geriatric medicine is a “whole person” specialty. Based on a solid infrastructureof general medicine, it involves consideration of psychological, social and spiritual dimensions, together with functional and environmental assessments. A geriatrician needs to be aware of legal aspects - capacity and consent, human rights, guardianship; and ethical conundrums, such as when to investigate or treat.
Professor Graham Mulley, Emeritus Professor in Geriatric Medicine, University of Leeds