Jane Murphy is Professor of Nutrition, Registered Nutritionist and Dietitian and co-leads the Ageing and Dementia Research Centre at Bournemouth University. Her research is committed to key nutrition-related problems in ageing and translation of nutrition science into practice. She also leads funded research projects on malnutrition in older adults and the complex problems faced by people living with cognitive impairments and dementia across the community. She is Clinical Lead (Nutrition) for the Healthy Ageing Programme, (previously Nutrition in Older People Programme) – Wessex Academic Health Science Network.
The context
Whilst improved life expectancy is to be celebrated, it is unfortunate that many older people will not live longer lives in good health because of poor nutrition. Malnutrition (as undernutrition) is a huge issue in the UK and becoming malnourished is a significant threat to our health as we age. Malnutrition is largely preventable and treatable and yet is a growing problem for our ageing population, often overshadowed by the health concerns of obesity.
Good nutrition is a basic right and yet around one-in-ten (about 1.3 million) older people over 65 years in the UK are malnourished or at risk of malnutrition and struggling to cope with everyday tasks of eating and drinking. Being malnourished has serious consequences resulting in reduced independence, delayed recovery, more frequent nurse and GP visits, more frequent hospital admission and increased length of stay. Despite national policy, NICE guidance and quality standards recommending nutritional screening using validated tools such as the ‘Malnutrition Universal Screening Tool’ (‘MUST’) in clinical settings, malnutrition remains under-detected and under-treated particularly in the community where we see the majority of older people with or at risk of malnutrition.
The cost implications are immense. In 2015, the management of malnutrition was estimated to cost at least £19.6 billion in England (£23.5 billion in the UK), which is about 15% of the total expenditure on health and social care, but likely to be much more today in real terms with inflation and population growth.1 It costs more to manage malnutrition than it does to manage obesity.2
These unprecedented financial challenges across health and social care mean we can no longer afford to ignore malnutrition. We need to become much smarter at identifying those at risk earlier and recognising symptoms early.
Working together
Over the past few years, it has been a great privilege to work with Kathy Wallis and the team at the Wessex AHSN. I have been Clinical Lead, formerly with the Nutrition in Older People Programme, and currently with the Healthy Ageing Programme (Nutrition). At Bournemouth University, my research interests have been committed to nutrition-related problems in older adults, especially those living with dementia. Working with the Wessex AHSN has provided a valuable opportunity to address malnutrition in older people but from new insights and perspectives. We have developed and established new relationships working with NHS Trusts, charities and other organisations including Age UK, The Patients Association, BAPEN and a range of staff and volunteers across the wider workforce and have engaged with new local and national networks.
The work has involved various projects to understand the barriers and enablers to nutrition screening in the community. Through this it has become evident that there was a need for new validated tools to identify malnutrition early and provide appropriate advice and signposting to help and support. Whilst much of the focus has been on disease-related malnutrition, the social causes including social isolation is often overlooked. Therefore the wider workforce in the community (including volunteers and carers) are in a better position to deal with this and integrate with health and social care staff as part of new pathways.
New tools
At the end of 2016, the Patients Association developed the original version of the Patients Association Nutrition Checklist. Working in collaboration, we developed it further and tested it across a range of settings including domiciliary care and the voluntary sector. The final version included two sections. Section A identifies risk (4 questions focussing on weight, unplanned weight loss, loose fitting clothes, poor appetite). For people identified at risk, section B provides guidance on simple advice, signposting, follow-up and resources.
We have also undertaken research to validate the questions in Section A against ‘MUST’. By using ‘MUST’ and the Checklist in 312 older people in lunch and activity clubs, our research showed that 9.9% of people were at-risk using the ‘MUST’ and 21.8% of people were at risk using the Checklist. Whilst there was moderate agreement, these key findings suggested that the Checklist could be used for early identification of malnutrition risk as it picked up people in the earlier stages of weight loss and with appetite changes. The research has been presented at BAPEN 2018 conference and will be published soon in the Journal of Human Nutrition and Dietetics. The Patients Association Nutrition Checklist was launched in December 2018.
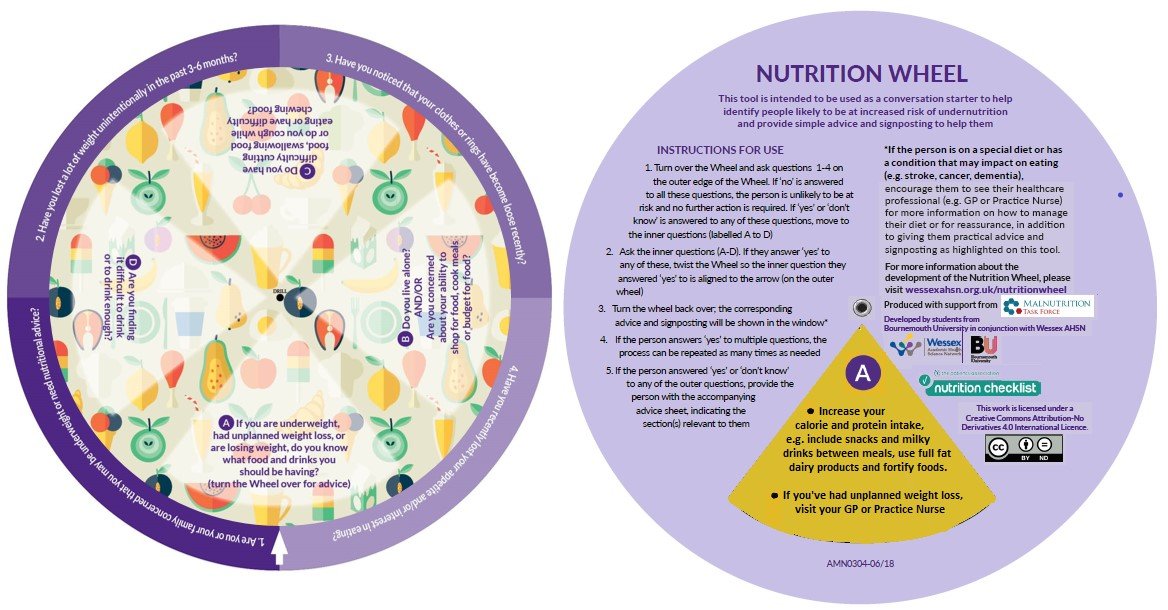
We have developed an interactive version called the ’Nutrition Wheel’ based in the Patients Association Nutrition Checklist. It is a conversation starter to help the wider community workforce to identify malnutrition and provide basic advice and signposting. This all started out as a prototype developed by an enthusiastic group of healthcare students from Bournemouth University in 2017. Further research followed to inform the design and usability and then to investigate the feasibility and acceptability of the Nutrition Wheel with volunteers in lunch clubs, activity and other community groups in Dorset, Hampshire and Hertfordshire.
A Nutrition Wheel Toolkit has been developed which includes the following:
- Advice sheet
- Explanatory Guide
- Nutrition FAQ
- Information for General Practice
- Development of the Nutrition Wheel
- ‘How to’ Video
This also includes the OPEN undernutrition leaflet which was developed by the Wessex AHSN as part of the Older People’s Essential Nutrition (OPEN) project. This leaflet is part of the Wessex AHSN OPEN toolkit. However other appropriate resources developed locally, can be used with the Nutrition Wheel.
The Nutrition Wheel could be used across the community in a variety of settings. Alongside lunch clubs, activity clubs, this could include day centres and events, waiting areas in GP practices, community clinics, community pharmacies, by Dementia Advisors, wardens in assisting living and housing communities.
Next steps
The Nutrition Wheel Toolkit was launched across the Wessex region and then at the Malnutrition Task Force on 23rd September 2019 as part of a new resource kit with the Patients Association Nutrition Checklist, PaperWeight Armband and BAPEN self-screening tool.
Final thoughts
More research is needed to understand how the Nutrition Wheel/Patients Association Nutrition Checklist:
- could be embedded as part of a new pathway for early identification of malnutrition and signposting in community settings
- could work together and support better application of clinical screening tools, such as ‘MUST’ to identify malnutrition and ’clinical concern’ (unintentional weight loss, loose fitting clothes, poor appetite) in the context of a conversation and signposting to appropriate nutritional guidance.
We also know that people who are malnourished are four times more likely to become frail. There is increasing awareness of the detrimental health impact of frailty on older people and high prevalence of malnutrition. Both frailty and malnutrition have been shown to result in similar negative health outcomes. Moving forward, work also needs to focus on how these conditions overlap to target interventions, provide new tools to improve treatment strategies for frail malnourished older people too.
So there’s still much work to do, but what we‘ve achieved to date represents a massive step forward in identifying risk of malnutrition quickly, simply and effectively. Hopefully it will start to remove the barriers and enable our older relatives to stay nourished, keeping them healthy and living at home for as long as possible and out of hospital.
UK Malnutrition Awareness Week 2019, taking place from 14-19 October, is a significant campaign to raise awareness of malnutrition (and dehydration) in the UK. Founded by BAPEN and the Malnutrition Task Force in 2018, the campaign seeks to increase understanding of this important issue among health and social care workers, community groups and the public, and mobilise people to take action to identify and prevent malnutrition. There are plenty of ways to get involved. Follow #MAW2019 on social media for more ideas.
Thanks for the opportunity to share our story and some of my thoughts. None of this would have been possible without working with a great team and amazing people across the community who have offered their valuable time and support to help us along this incredible journey… but it’s not ended yet!