Dr Abi Hall is a clinical academic physiotherapist based at the University of Exeter, specialising in the rehabilitation of older people. She is a co-author of the Age and Ageing paper Behaviour change interventions to increase physical activity in hospitalised patients: a systematic review, meta-analysis and meta-regression. She tweets as @abijhall.
In early 2020, as an early career researcher, I was given the exciting opportunity to join an international collaboration to undertake a systematic review, an opportunity that was too good to turn down. The collaboration involved other researchers in the UK from the Universities of Exeter and Hertfordshire and in Australia at La Trobe University - all with a variety of skills and experiences, but with one thing in common – a passion for physical activity.
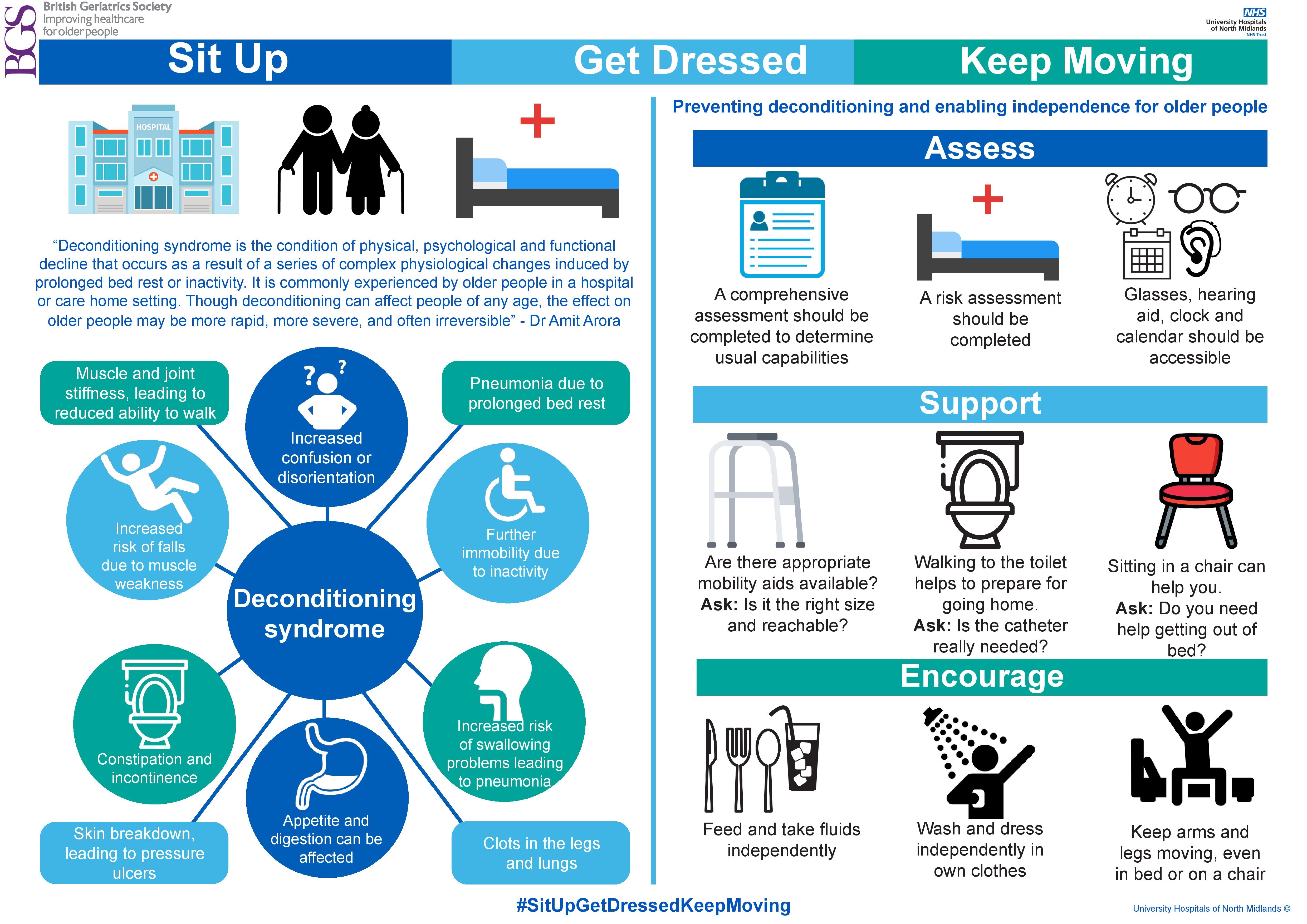
With #EndPJparalysis becoming a global drive, there is growing recognition that lack of physical activity during hospital stays can have significant negative consequences for patients, especially in older people. People in hospital massively reduce their activity levels with some studies reporting that hospitalised older people only move an average of 400 steps per day! There is an abundance of evidence that suggests lack of activity in hospital leads to reduced functional ability, deconditioning, as well as worsening of cognition. These are all major factors that can prevent discharge and increase reliance and pressure on social care. A key problem is that despite the evidence to suggest that lack of activity in hospital can worsen outcomes, there is little evidence to suggest what strategies are effective to prevent or reduce this problem. A key issue is the recognition that physical activity is a behaviour, suggesting that attempts to increase physical activity should be based on behaviour change techniques. Indeed, the aim of this recently published systematic review was to determine if behaviour change interventions are effective in increasing levels of physical activity in hospitalised patients. Secondary aims explored the effect of behaviour change interventions on patient outcomes, health service outcomes, safety and the patient experience and the association between specific behavioural change techniques and increased physical activity in hospitalised patients.
The review included 20 randomised controlled trials, which studied a total of 23 behaviour change techniques such as goal-setting, feedback on performance and instructing on how to perform a behaviour. It comprised four trials on stroke wards, fourteen involving acute wards and six on rehabilitation wards. The review found evidence to suggest that behaviour change interventions can result in increased physical activity among older hospitalised patients, however there was inconclusive evidence to suggest changes in mobility. Our results demonstrated that goal-setting and feedback were the behaviour change techniques that worked best to increase physical activity.
As an early career researcher, for me the opportunity to see all stages of a large systematic review from development to publication, while collaborating with a large international team, was a real eye-opener and a valuable experience. It also gave me the chance to expand my network of researchers with similar research interests.
Read the Age and Ageing paper Behaviour change interventions to increase physical activity in hospitalised patients: a systematic review, meta-analysis and meta-regression.