Foreword
The BGS has long advocated for a better staffed healthcare workforce to care for the needs of the UK’s rapidly ageing population. Workforce pressures are nothing new and it is well known that the NHS is experiencing severe staff shortages. As a result, healthcare workers report feeling exhausted. These challenges are exacerbated by the failure to resolve long-standing industrial disputes. There is a long way to go to solve these problems. Concerted action is needed to recruit more healthcare professionals into the specialty of geriatric medicine, especially to rural and coastal areas where the populations are likely to age faster, and to retain and support existing staff.
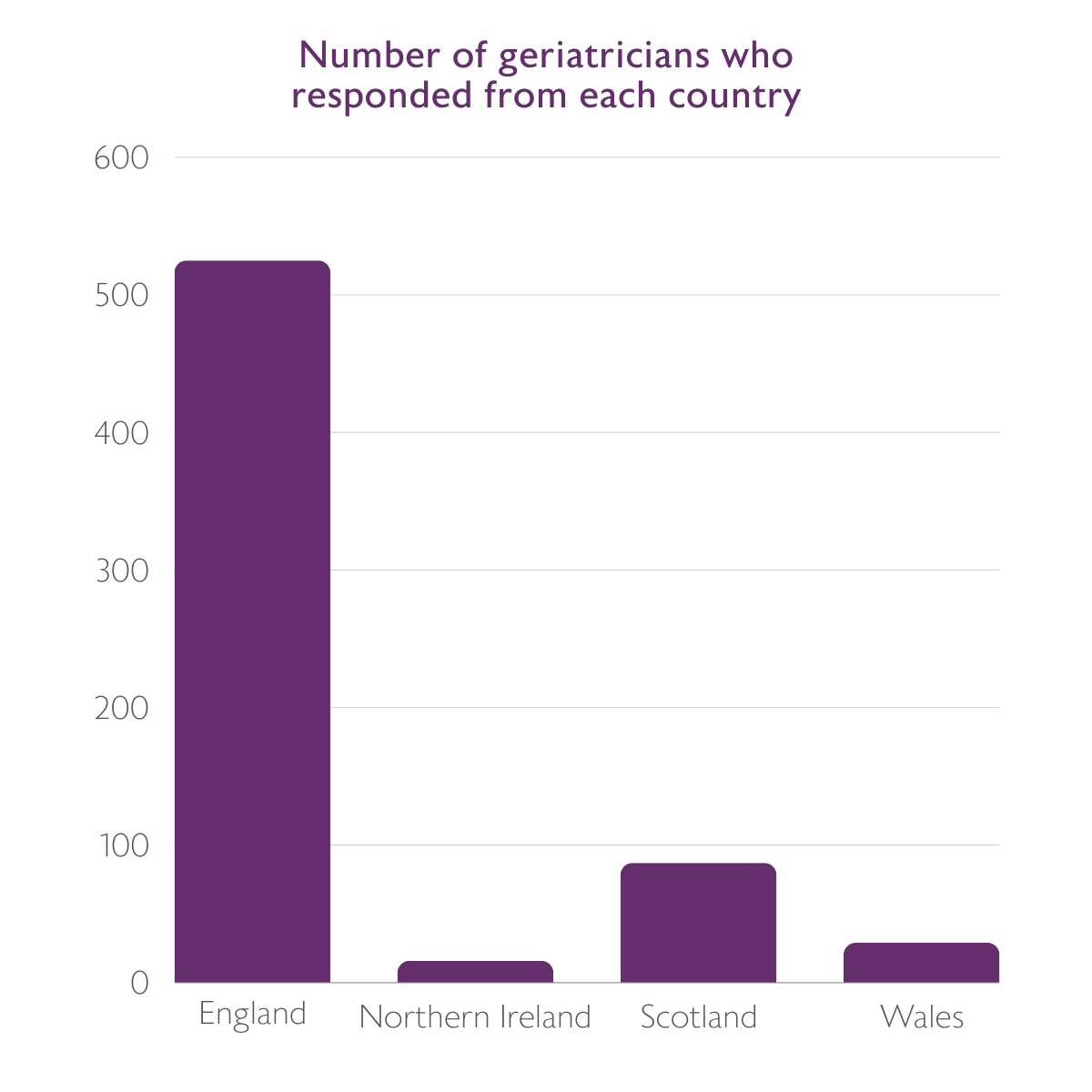
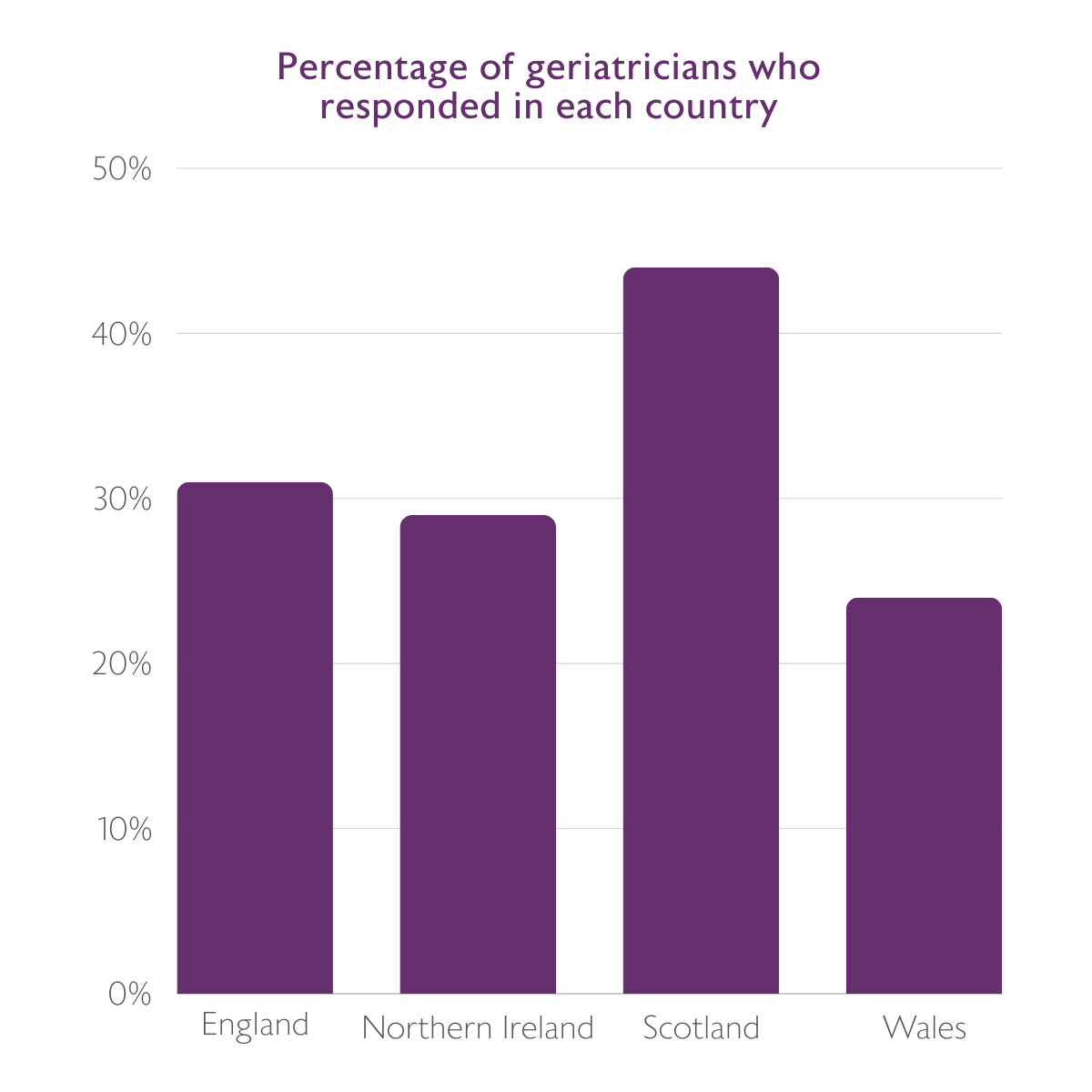
This report analyses data from the UK 2022 census of consultant physicians conducted by the Royal College of Physicians (RCP) on behalf of the RCP London, the Royal College of Physicians of Edinburgh (RCPE), and the Royal College of Physicians and Surgeons of Glasgow (RCPSG). The census was published in 2023, using data that was collected in 2022. The BGS would like to express thanks to the RCP who work to conduct this annual census. The data is a valuable resource that allows us to keep track of the current state of the consultant workforce caring for the older population. Of course, consultant geriatricians are just a small part of the multidisciplinary workforce that provide healthcare to older people. The BGS will continue to seek data on the wider workforce in our endeavour to represent the whole multidisciplinary team. Our recent report, The state of the older people’s healthcare workforce: A report from the BGS membership survey, captures some of this evidence from our wider membership but more high level data is needed.1
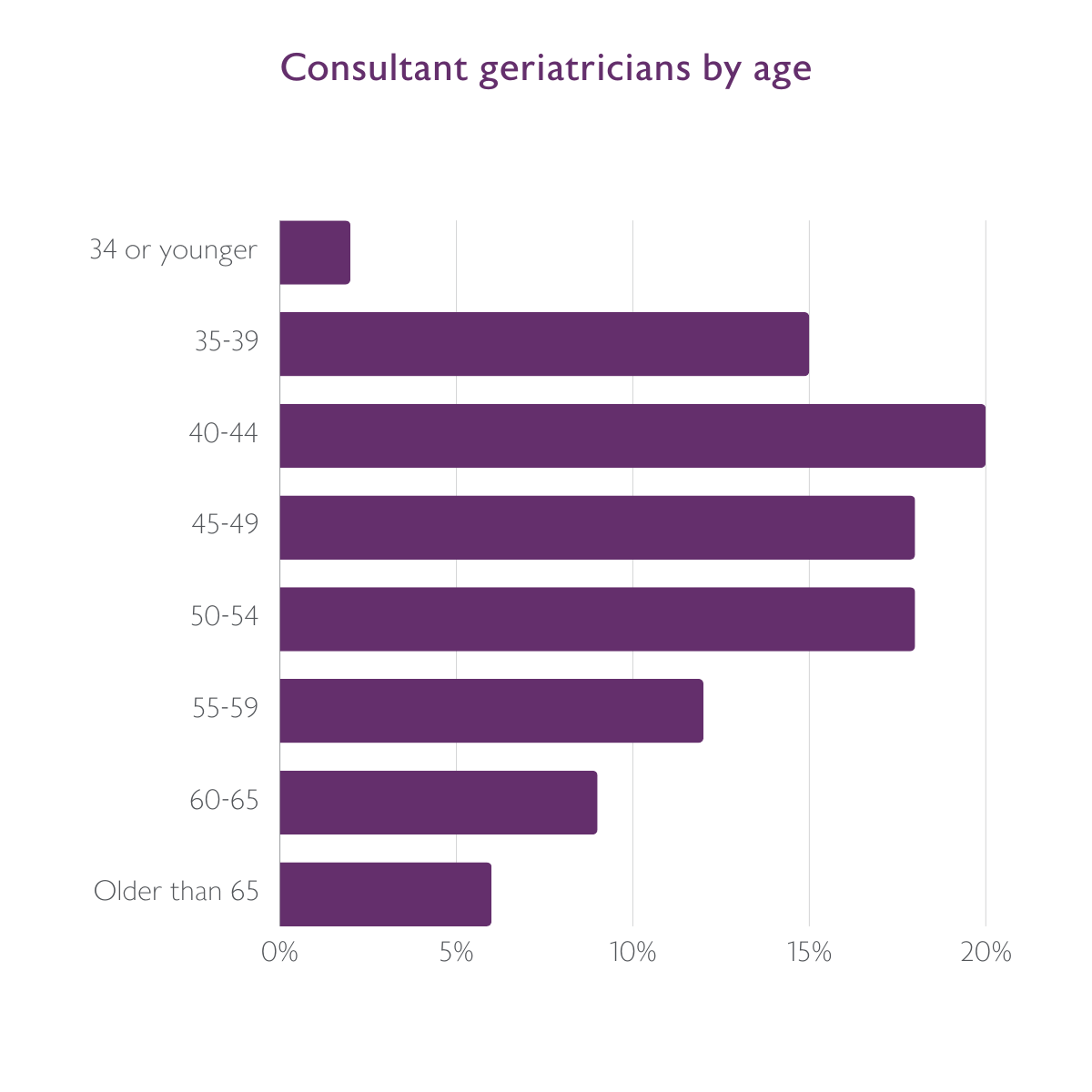
Nine months on from the publication of The Case for More Geriatricians: Strengthening the workforce to care for an ageing population,3 the new census data highlights that there is still a long way to go to meet our calls and make up for the shortfall in consultant geriatricians. The current shortage is only expected to worsen, with just under a half of geriatricians expected to retire in the next decade and more people needing healthcare in their later years. The report also highlights that there is an uneven geographical distribution of geriatricians in the UK, with urban areas typically being better served despite the ageing population more likely to be found in rural and coastal areas. On the ground, most geriatricians report substantial staff shortages and do not feel in control of their workload. These frustrations echo the findings of our recent membership survey which painted a bleak picture of the wider workforce and highlighted that staff shortages have a big impact on mental and emotional wellbeing of healthcare professionals.1
Despite frustrations, most consultant geriatricians are happy with the specialty of geriatric medicine, and we know many of our members find their roles rewarding. This sentiment needs to be captured in a recruitment drive, starting to build increased training numbers. We are excited by our own upcoming #ChooseGeriatrics BGS campaign which will promote the specialty to medical students and the wider multidisciplinary team, making the case for the older people’s healthcare workforce. More information on this campaign will be publicised soon and we would value support from BGS members and others.
As the biggest users of the health and social care system, older people’s needs must be at the centre of workforce planning. The upcoming general election is a vital opportunity for political parties to consider the needs of an ageing population and the workforce supporting it. Health policies must address current staff shortages and put geriatricians where they are needed most. This is vital so that, across the country, older people can receive high-quality, personalised care, now and in the future.
Professor Adam Gordon
BGS President
Dr Amit Arora
BGS Vice President for Workforce