End of Life Care in Frailty: Introduction and Foreword
Introduction - Dr Eileen Burns MBE
Most of us will die in old age, and currently many of us will not have been prompted or given the opportunity to reflect on our wishes regarding the end of our lives.
Where do we wish to die? As we perhaps develop frailty, how do we wish our doctors, nurses and other care givers (including family members and friends) to respond to our needs?
Will the healthcare we receive be appropriate and in keeping with the optimisation of our comfort, with an overt recognition that we are coming to the end of our lives?
In society and healthcare today, death is often seen as a failure, and yet we will all die."
Too often the clinical response to an acute deterioration in a frail older person is a protocol or pathway-driven move into an invasive - and sometimes distressing - interaction, without pause to reflect on the values of the older person.
What is their understanding of their current situation? What is their preferred approach? Good end of life care cannot be provided by a single service or indeed by healthcare alone, as it involves the person, their family, their friends and carers and the cultural context in which they have lived and wish to die.
At all times we must strive to put the person at the centre of our decision-making and construct services to suit them not us.
The aim of this document is to support clinicians and others in considering the needs of and providing high quality care for frail older people as they move towards the end of their lives. It aims to prompt and support timely discussions about preferences for care, ideally at a time which facilitates the input of the older person themselves.
If the older person lacks capacity, the section on ethics and law in this area provides clarity as to who must be consulted and the principles which guide decision making.
Uncertainty is frequently present in prognostication for frail older people. We may have evidence that this person belongs to a group of individuals for whom there is a 50% likelihood of death within the next 6 or 12 months, but such tools cannot accurately identify the risk of death for any given individual.
Good end of life care cannot be provided by a single service or indeed by healthcare alone, as it involves the person, their family, their friends and carers and the cultural context in which they have lived and wish to die. "
Many of us will be familiar with the conversation with a family regarding the uncertainty of outcome and risk of proximity to death when a family may tell us that this is the third or fourth time a doctor has told them their mother is likely to die. However, older people themselves tell us they value honest open communication with a recognition of uncertainty when it exists.
Recognition of severe frailty is an indicator that consideration of the wishes of the patient regarding their care and advance care planning (if not already commenced) needs to begin. Patients with severe frailty have a high risk of death within the next 6 months. Higher risk of death is seen in frail patients in the community (whether within their own homes or living in care homes), and in acute hospital admissions. Thus, recognition of severity of frailty is an essential complementary part of identification of risk of death.
There has been a huge growth in the literature on frailty over the last 10 years. Patients presenting with falls, 'off legs' and delirium are frequently living with frailty. These patients are often prescribed multiple medications with high risk of adverse drug reactions. They are at increased risk of unwanted effects of an acute hospital stay (inpatient delirium and falls, pressure injury, malnutrition and incontinence).
Too often the clinical response to an acute deterioration in a frail older person is a protocol or pathway-driven move into an invasive - and sometimes distressing - interaction, without pause to reflect on the values of the older person."
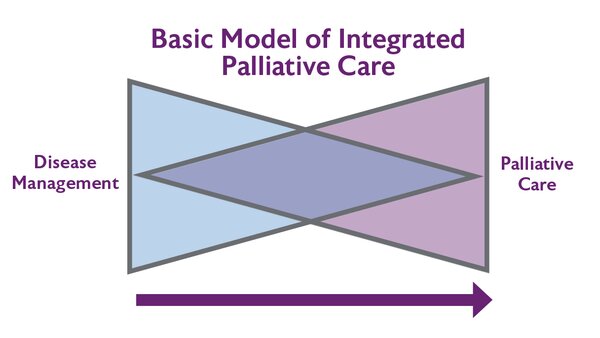
The disciplines of geriatric medicine and of palliative care share many of the same values and aims. Both are firmly rooted in person-centred care and both aim to improve quality of life for the recipient of care, utilising the skills of a multidisciplinary team. Comprehensive assessment, case management and collaborative working are core to both.
Geriatric medicine strives to restore and optimise function, especially after an acute deterioration. In palliative care more emphasis is laid on symptom control and the alleviation of psycho social distress and spiritual concerns. Integration of the skills of both areas with the aim of enabling the older person to live as well as possible, with the highest level of independence and with optimisation of management of troublesome symptoms provides the best opportunity for the maintenance of physical and cognitive function and autonomy (including important decision making around end of life care) for as long as possible – where possible until the time of death.
We hope to bridge the gap between geriatric medicine and palliative care and to address the particular issues which may affect older people dying with frailty - some of which may not be considered part of the usual remit of either specialty.
The care of older people in the last phase of their lives is provided by a wide range of individuals. Spouses and other family members, supported by district nurses and GPs, are often the main providers of care. Specialists such as geriatricians and palliative care consultants working in multidisciplinary teams may also have a significant role within the community, hospital or hospice settings.
The aim of this guidance is to provide practical advice to help those staff working with frail older patients so they can provide their patients with the best opportunity to live and die well.
- Dr Eileen Burns MD FRCP(London), FRCP(Ed) MBE
Consultant Physician
Past President, British Geriatrics Society

Foreword - Dr Sarah Russell RGN
Death is inevitable, but how we live and die is not.
As life moves on towards its inescapable end, we live... with the knowledge of our inevitable death. "
The twists and turns of frailty are a familiar companion."
The guidelines provide practical, relevant, evidence based recommendations, while keeping the person at the heart of it. I commend them to you.
- Dr Sarah Russell RGN
Family Carer, Professional and Practice Development Facilitator, Dementia UK;
Non-Executive Director, End of Life Integrator and Contributor, Lancet Commission into The Value of Death