What is frailty?
- An inevitable consequence of ageing
- A state due to multiple long term conditions
- A condition in which the person becomes fragile
- A state associated with low energy, slow walking speed, poor strength
- A condition for which nothing can be done
Answer: 4 - low energy, slow walking speed, reduced strength
So the other are untrue-
- not inevitable,
- associated with multiple LTC, but can occur in the absence of these
- amenable to treatment
- unlike “fragility” frailty is a specific syndrome with characteristic features, and a rapidly expanding research base
Frailty: why is it important
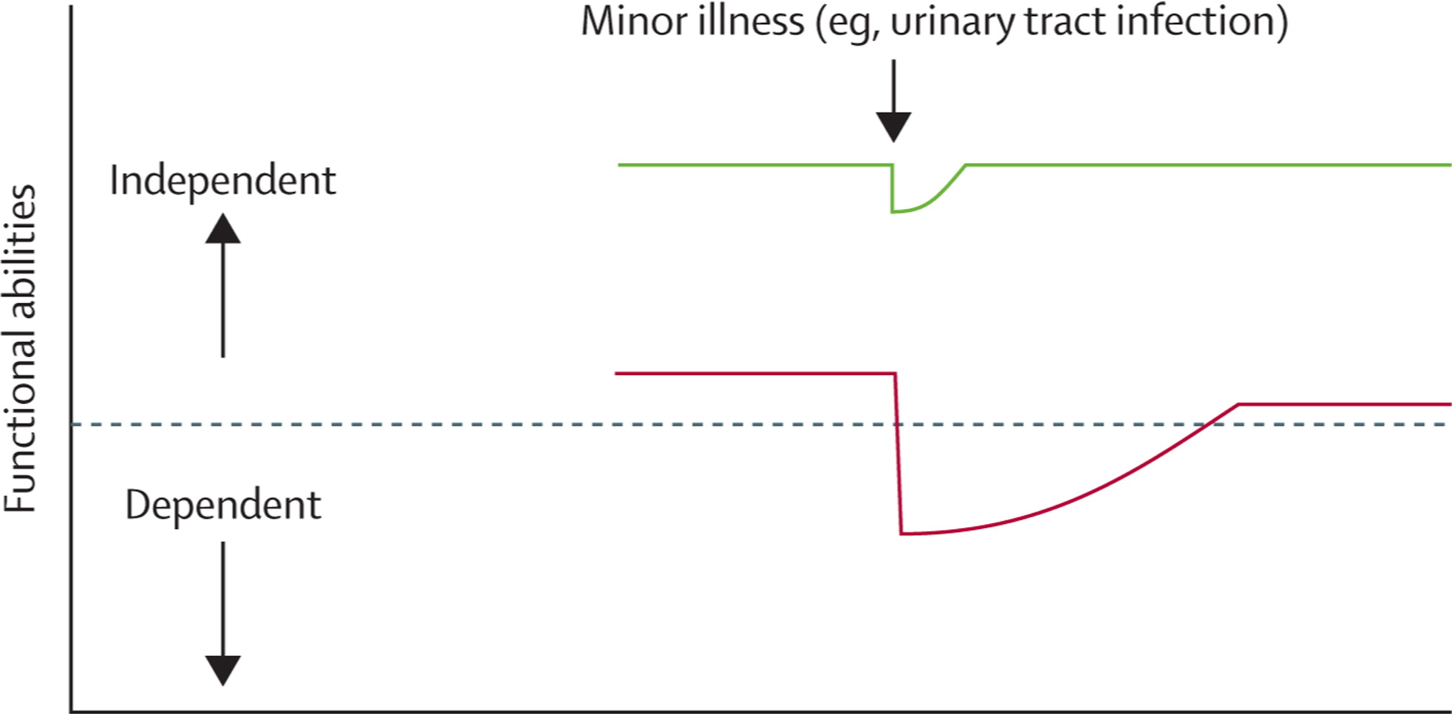
Definition: a state of increased vulnerability to poor resolution of homoeostasis after a stressor event
Condition associated with increased risk of deterioration:
- “acute frailty syndromes” – falls, delirium (or acute confusion), “off
- legs” may result from a relatively minor insult
- Higher risk of acute hospital admission
- Care home admission
- Death