This is chapter 2 of a series. See the full series here.
These are valid plans that may lead to improvement. However, you should consider the evidence which has consistently shown that care for frail older people in non-geriatric acute care settings is better when assessment and management of frail older patients is integrated into the whole service (see Box 4).
|
Evidence suggests that integrating assessment and management of frail older patients into your service is a more effective way of organising care than having a consultation geriatric service at arm’s length. (2) Greater effectiveness relates mainly to joint decision making and shared control over patient identification and treatment by geriatric and non-geriatric expertise. “It’s very nice doing joint ward rounds, [geriatricians and surgeons,] because you end up with lots of two-way education, a lot more understanding of where each of us is coming from, and I think it’s just very good for the patient to see that we are working together, and that we are making joint decisions, together with the patient, and providing them with that more overall information which is what the patients want rather than it being purely about the surgical complications.” (Consultant Geriatrician) "Because for the nature of CGA you can't have it as a liaison because of it being such a team approach and you need the team that you are working with to be working together with you with the shared vision. You can't have liaison." (Geriatrician) |
To give you a better idea of what organisational change may be needed, we have developed a self-assessment tool. It will allow you to compare existing service provision to what gold-standard care for frail older people should look like in an acute care setting. This way it will help you to identify service-level competencies already in place as well as any gaps that will need to be addressed in planning organisational changes to integrate assessment and management of frail older people as part of your service.
When you open the self-assessment tool (see Appendix 1 - downloadable from the sidebar), you will find it has two parts.
- First it assembles key service-level competencies that together ensure high-quality care for frail older patients, and prompts you to check whether they are routinely available in your service.
- Second it offers evidence-based tools and actions to fill gaps in those competencies.
You may be able to answer some of the questions in the toolkit straight away. However, there may be areas where you are not sure about how your current practice looks. For some of the questions, it may be that you have local policies and protocols in place, but they are inconsistently followed in practice. We suggest taking time to complete the self-assessment tool, rather than seeking to complete it instantaneously. Discuss the questions with your colleagues in your team to gain their views on the strengths and weaknesses of current practice, and consider undertaking reviews (e.g. PDSA style measurement) of current practice (for example, via case notes), particularly where you are not sure whether things are being done consistently, or where you suspect there may be a gap between the existence of a local policy and what actually happens.
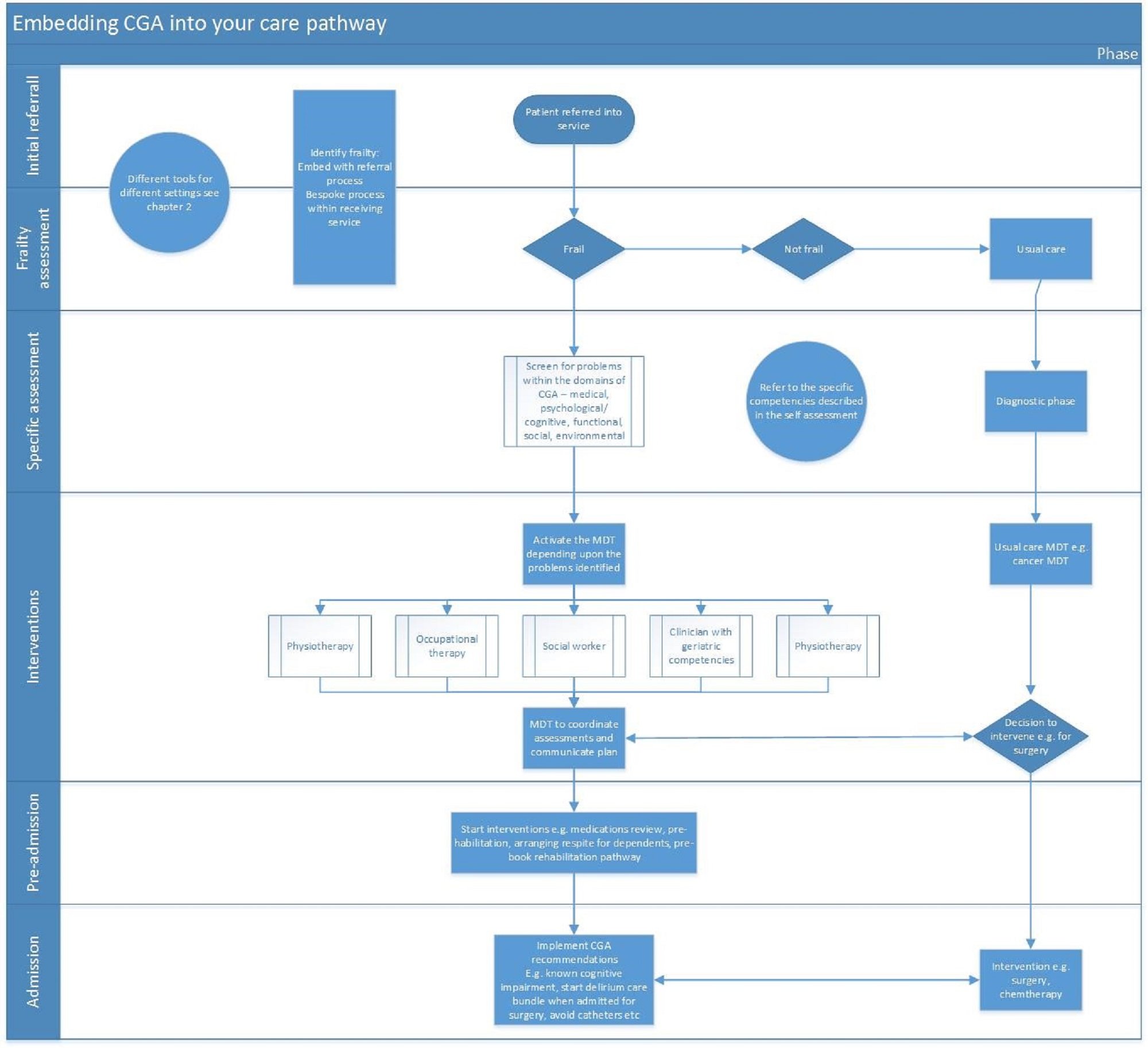
To help you start to think about the aspects of your service that need reviewing, Figure 1 provides a schematic representation about how CGA might be embedded into a service (in this case a cancer service, but the principles should apply more broadly). You will see that there are key points that need testing to determine if they are in place already or nor, for example, frailty identification, screening for geriatric syndromes, involvement of the geriatric (as opposed to cancer Multidisciplinary Team (MDT)), communication and coordination in an MDT meeting etc.