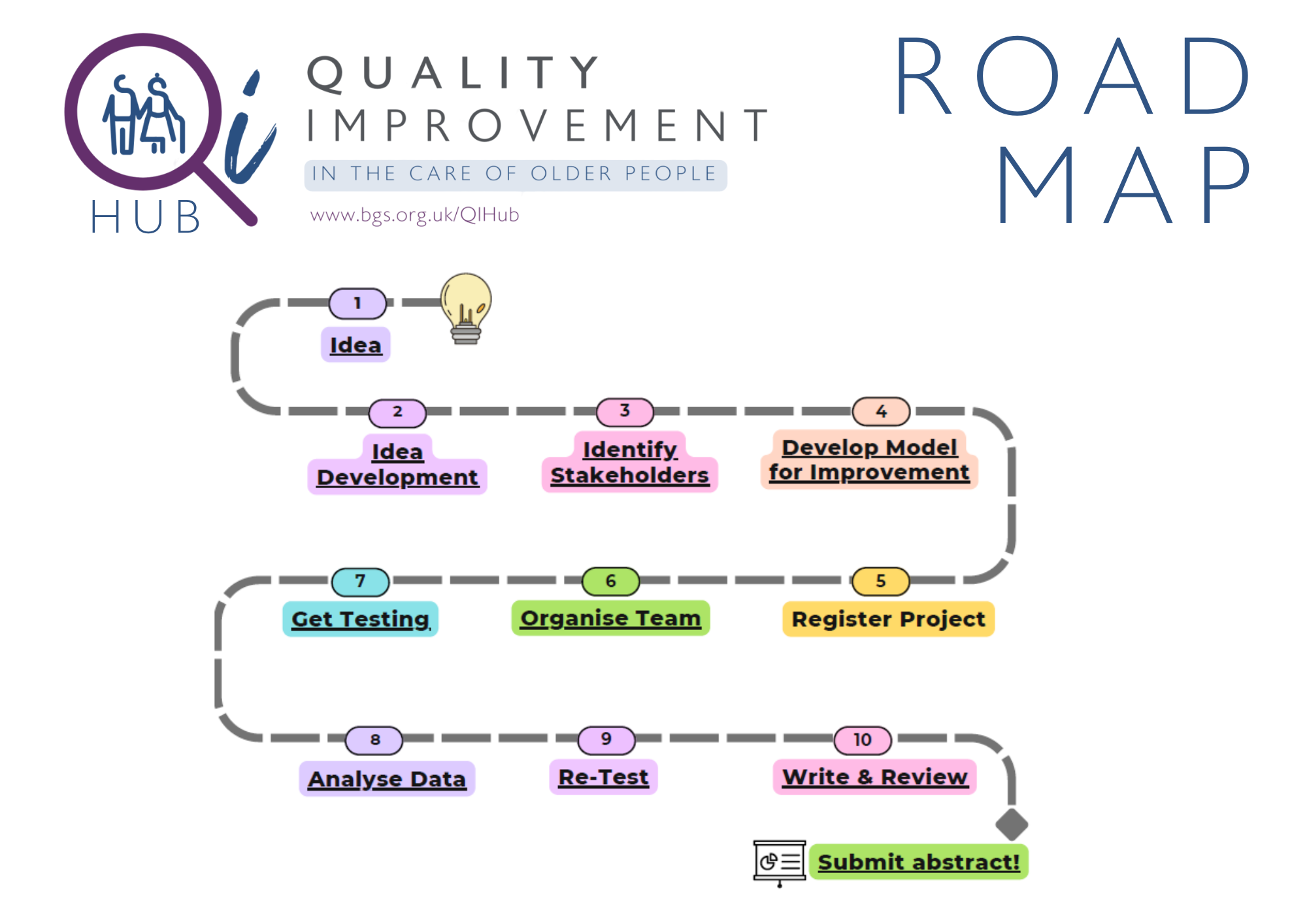
Ideas for QI projects relevant to older people
If you are struggling for ideas about where to start on your Quality Improvement journey, below are a few suggestions to get you started. We hope the ideas below act as a springboard for your project - and if in doubt, speak to your team!
|
Preventing harm |
Patient Safety |
Implementing best practice |
Working with patients and carers |
|---|---|---|---|
|
Preventing Constipation |
Falls Risk Assessment |
Introducing Comprehensive Geriatric Assessments |
Advance Care Planning |
|
Contracture prevention |
Fragility Fractures: Risk assessment and management |
Identifying Delirium |
Understanding and Reducing Carer Stress |
|
Fluid intake and restriction |
Improving Medication compliance: e.g. Reducing missed medications on chart |
Dementia Care: Referral to CNS, Carer Passports |
Correcting sensory impairment: Hearing aids, glasses etc. |
|
Diarrhoea: Managing Infection vs. Overflow |
Pain assessment and management |
Mood assessment and treatment |
DVLA Driving Advice |
|
Incontinence: Managing Urinary and Faecal incontinence |
Postural Hypotension |
Parkinson’s: e.g Inpatient CNS review, medication timing |
Planning for End-of-Life Care |
|
Nutrition assessment: MUST, Food & Fluid charts |
Perioperative anticoagulation |
Safe Sedative use: Z-Drugs, sedatives, benzodiazepine, |
Providing Family Updates |
|
Improving and maintaining Oral health |
Treatment Escalation Plans |
|
Preventing PJ Paralysis |
|
Assessing and reducing Polypharmacy |
Reducing opiate use |
|
Sleep |
|
Preventing Pressure sores |
Improving Communication and hand-over |
|
Improving Communications |