Overview
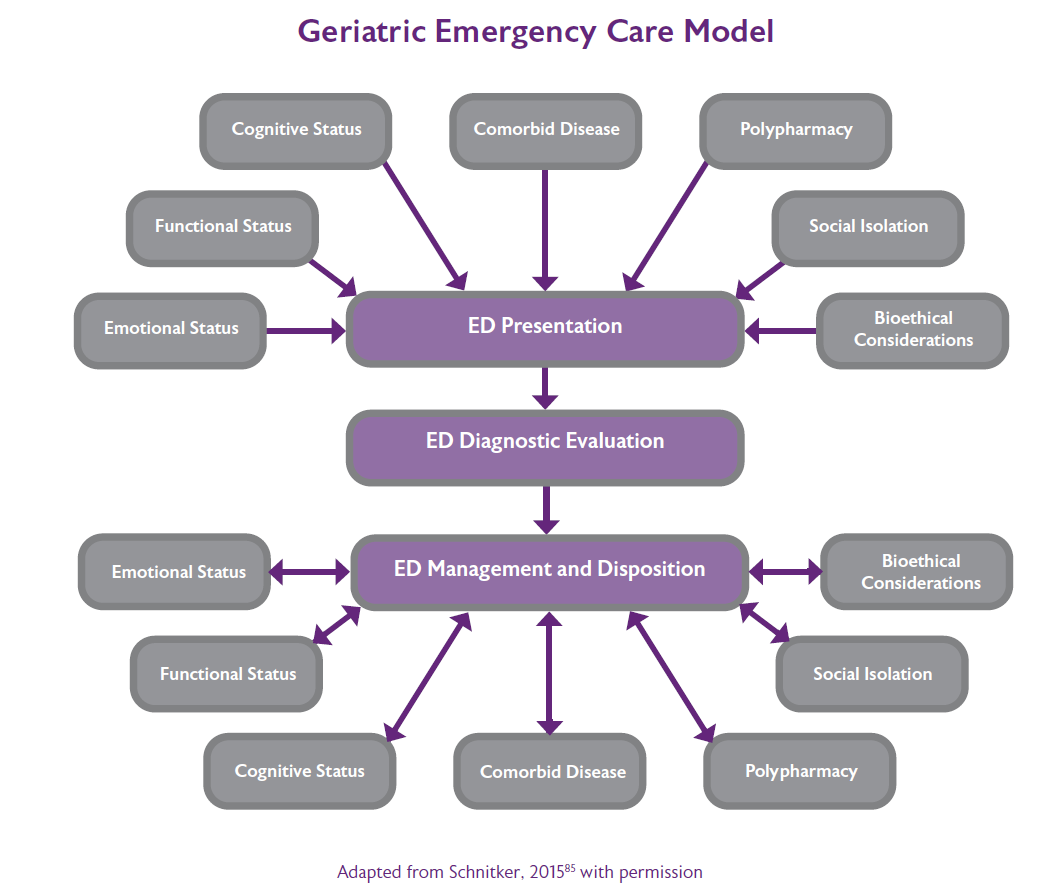
More and more, older people are the major patient group in the context of urgent care scenarios, whether in the acute hospital or in the community. Many older patients living with frailty suffer from a complex combination of multiple diseases, often combining mental, physical and social impairments, yet services are often not designed with these complex needs in mind.
- A quick overall review of the complexity of the case (using for example the Clinical Frailty Scale45), taking into account the medical and psychosocial history, vital signs and symptoms
- Shared goal setting fitting the urgency and the stage of life (i.e. aiming for cure or recovery vs. palliative or end of life care
- Determine the approach and interventions that can serve this goal
- Shared decision making to generate a management plan that best fits the individualised personal goal and has the best balance of added value versus risks and burden
- Reflection on action, to assess the benefit, and to learn together as acute care team.